Abstract
Background
Health economic evaluations require cost data as a key input, and reimbursement policies and systems should incentivize valuable care. Subfertility is a growing global phenomenon, and Dutch per-treatment DRGs alone do not support value-based decision-making because they don’t reflect patient-level variation or the impact of technologies on costs across entire patient pathways.
Methods
We present a real-world micro-costing analysis of subfertility patient pathways (n = 4.190) using time-driven activity-based costing (TDABC) and process mining in the Dutch healthcare system, and built a scalable and granular costing model.
Results
We find that pathways (13.203 treatments, 4.190 patients, 10 years) from referral to pregnancy and birth vary greatly in costs (mean €6.329, maximum €36.976) and duration (mean 25,5 months, maximum 8,59 years), with structural variation within treatments (and DRGs) of up to 65%. Patient-level variation is highest in laboratory phases, and causally related to patients’ cycle volume, type, and treatment methods. Large IVF or IVF-ICSI cycles are most common, and most valuable to patients and the healthcare system, but exceed their DRGs significantly (33%). We provide recommendations that reduce costs across patient pathways by €1.3 m in the Netherlands, to support value-based personalized care strategies. These findings are relevant to clinics following European protocols.
Conclusions
Fertility treatments like IVF feature significant cost variation due to the personalization of treatments, and rapidly evolving laboratory technologies. Incorporating cost granularity at the patient and treatment level (cycle volume, type, method) is critical for decision-making, economic analyses, and policy as both subfertility rates and treatment demand are rising.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
Healthcare providers are highly complex organizations that deliver increasingly tailor-made procedures, treatments, and services. In the case of complex care like fertility care, such treatments draw on a variety of costly medical specialties, and use expensive equipment and materials to different degrees per patient [1]. Accordingly, “managing and financing healthcare services requires a detailed understanding of how resources are used” [2], for which European countries use Diagnosis-Related Group (DRG) prices as unit cost estimates [3, 4], input for reimbursement negotiations (e.g. The Netherlands, Germany, France), or as descriptive instruments to inform policy or budgets (e.g. Nordics).
However, in complex care settings such as fertility care, DRGs may offer insufficient granularity to support comparisons or decision-making within treatment categories [5,6,7,8]. This does not present an issue to reimbursements, if the DRG covers the average costs of care, but DRGs alone may be insufficient to pursue value-based care strategies and/or discover process (in)efficiencies or cost differences between patient groups, alternative technologies, or alternative pathways within treatments [2, 9, 10]. For example, the current Dutch DRG for one in-vitro fertilization (IVF) with intra-cytoplasmic sperm injection (ICSI) treatment is €3.064 (14B168), even though European clinics offer varieties within this treatment type, which require different resources, and which clinics are unaware of due to lacking cost estimation infrastructure [11]. In this study, we find this treatment to vary significantly in clinician time spent and costs (by 65%; €2.479 to €4.089), and these differences structurally relate to patient-level characteristics, such as the number of embryos cultured, and the number of consultations required. Additionally, the construction of DRGs has featured significant variation in how indirect costs are allocated to treatment categories [2, 10, 12, 13], which is challenging in complex care settings like fertility care which utilize expensive specialized laboratories worth upwards of €1 m and thus feature significant indirect costs—excluding or underrepresenting indirect costs distorts economic analyses and decision-making [2, 14, 15]. Due to lacking cost estimation in hospitals [11], and due to the aggregate nature of Dutch DRGs in fertility care specifically [16], there is a general lack of understanding of how resource use varies across treatment types [17]. This currently poses a barrier to medical managers and policymakers that wish to assess medical technological advancements that improve the costs and outcomes within treatment types [12, 16], or across entire patient trajectories [18], as current DRGs cannot provide such opportunity cost information [1, 2, 7, 8]. Further, high profit margins and the use of lucrative ‘add-ons’ to attract vulnerable patients distort prices in countries like the US [19].
Subfertility is an escalating global epidemic; its global economic burden is predicted to reach 2 million treatment cycles per annum [20] at US$27 bn by 2026 [1, 21]. Subfertility impacts one in six individuals [22], so approximately 48 million couples and 186 million individuals worldwide [23], or 11% and 15% of US and EU residents respectively [1, 24, 25]. Consequently, identifying cost variation and savings across the patient pathway, and within broad treatment categories like IVF, is considered imperative to make treatments accessible to all [22, 26, 27], and to enable systematic cost reductions by implementing strategies like value-based healthcare (VBHC) [26]. This paper reports the implementation and findings of a comprehensive micro-costing project in the Dutch healthcare system. The aim of this study is to develop fine-grained cost insights in fertility care, to measure and improve costs and duration (time-to-pregnancy), by informing comparisons between technologies and treatment protocols within treatment types/DRGs, and across entire patient pathways from initial consultation to pregnancy.
The costing infrastructure developed in this project, informed by our protocol [16], is included as supplementary material for modification or use in other clinics or settings implementing VBHC. We discuss what our findings may mean for the use of DRGs in complex care settings, and how fertility treatments can be made more valuable to patients, clinics, and the healthcare system. For instance, our analysis indicates that employing vitrification techniques results in savings of up to €1.998 per pregnancy trajectory (across repeated treatments) and €1.311.396 in Dutch clinics, which may also be relevant to other European clinics following similar protocols. These savings result from the high frequency of repeated treatments per patient and the reduced workload due to clinical decisions made in earlier treatments that carry over to later ones.
Setting, method, and data
Setting
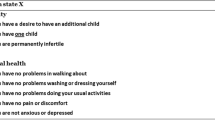
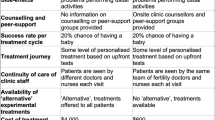
Patients diagnosed with subfertility need medical assistance to conceive and have children; various treatment options are available, and most patients undergo multiple cycles of month-long treatments on their journey from desiring a child to achieving pregnancy [5]. In Europe, all clinics or hospitals offering fertility treatments follow treatment protocols published by the European Society of Human Reproduction and Embryology (ESHRE). The Netherlands features mandatory basic health insurance that covers unlimited cycles of two kinds of subfertility treatment, namely ovulation induction (OI) and intra-uterine insemination (IUI), three cycles of in-vitro fertilization (IVF) or IVF-ICSI per live born child, and an unlimited number of frozen embryo transfers (FETs). If a couple wishes to pay for IVF or IVF-ICSI out of pocket (e.g., a fourth cycle, not covered by health insurance), this costs the DRG amount, namely €2.955 (14B168) or €3.064 (14B168) respectively, as per 2023. IUI treatments are reimbursed €737 (14B191) per cycle, and OI treatments are reimbursed €845 (14B192) regardless of type. FET, which are only possible after IVF treatments if embryos are cultured and frozen for future use, are reimbursed €817 (14D226) [28]. Within IVF treatments, FET cycles are most common, as shown in Table 1 depicting the most recently available statistics of Dutch and European treatment cycle types [29, 30]. In the Dutch setting, expenditures have risen significantly in recent years, and governmental agencies are attempting to reduce annual expenditure growth [31].
Study design
We apply a unique methodology described in the study protocol [16], which combines time-driven activity-based costing (TDABC) with process mining using data from one representative clinic which follows European protocols, to generate unique cost estimates per patient based on actual resource consumption, from initial consultation to pregnancy. TDABC uses the time spent by clinicians to allocate direct and indirect organizational costs such as equipment used, or salaries paid, first to treatment types and then to patient journeys by generating cost estimates that reflect individual patient-level variability through cost equations [16, 32]. The amount of time required can depend on cost predictors (e.g. number of ultrasounds), which results in per-patient variation in costs. In this way, TDABC uncovers the sources of cost variation, and allocates all yearly costs of running an organization such as a fertility clinic to treatment pathways by treating them as dynamic cost objects [32,33,34]. We first determine activity and process durations per treatment type, before simulating the estimation using longitudinal data through process mining. Per-patient costs are calculated by multiplying resource-specific capacity cost rates (CCRs) with durations, per cycle of care delivered, thereby incorporating patient-level variation in both direct and indirect cost allocation. The construction of these systems is subject to user design, i.e., the process of conducting TDABC cannot be standardized [12, 35,36,37,38], as the system can be made as fine-grained or broad as desired. This choice is reflected in the number of cost equations constructed, the number of patient parameters included, and the granularity of the CCRs. For example, some studies generate only a single CCR for an entire department [39], whereas others acknowledge different utilization rates within departments [33], and some include indirect costs whereas others exclude these [18]. For these reasons, such studies must be reported transparently, by reporting the CCRs generated, and the activities included and costed in each cost equation [38, 40].
To generate fine-grained cost estimates that are both accurate and generalizable, we used a detailed approach based on measured variation through participant observations during which the researcher shadowed clinicians and timed their work durations [40]. In doing so, we constructed cost equations that distinguish variation within treatment (and thus DRG) categories, by differentiating between different ways of working, and patient-level variation, within treatment categories.
Method and data
To estimate the costs of treatment cycles we measured the time required to deliver care, per staff function, per activity, for each treatment option. The study was conducted at the fertility clinic of the Reinier De Graaf Gasthuis hospital. To ensure accuracy [40], we documented care activities in chronological order using the Panton Metro Line tool [41], to establish transparency regarding which activities are costed. Each activity (e.g., a consultation, a diagnostic test, a procedure) is shown on the metro line, which forms a long chain of activities, and corresponds to an activity in the costing tool built in this project. These activity maps are based on treatment protocols, EHR data of all patients ever treated in the Dutch clinic since 2014 (n = 6.822), and healthcare professionals (HCP) input provided iteratively over one year. Due to the high data requirements of this method, and the high research burden of conducting observations and developing the medical metro line, we conducted the analysis at one Dutch clinic following ESHRE standards. To ensure generalizability, we chose a Dutch clinic that offers each treatment option, follows strict European protocols defined by ESHRE and NVOG [16, 42], and that operates as a financially and physically separate entity from a hospital. This allowed us to incorporate all variable overheads [40]. Further, the results were presented to four other Dutch fertility clinics for validation. To enable generalizability over time as embryology develops, we include the entire medical metro line and the editable costing tool in the supplementary appendix.
Next, we used participant observations over the space of one year to measure activity durations and identify sources of variation to determine cost predictors [33]. All participants observed and timed were asked for informed consent, following the study protocol [16]. To limit research burden, we used direct observations only in cases where activity durations could not be reliably estimated from scheduling data. For example, consultations always required 30 min of gynecologists’ or clinicians’ time and were therefore costed at a median of 30 min. Consultations occurring outside the clinic in another specialty, e.g., urology, were also observed, and activities exhibiting a large degree of variation in duration were observed more frequently (details are provided in the supplementary appendix).
Subsequently, cost data such as variable overheads [40], equipment purchase prices and disposables were inventoried and allocated to care paths using CCRs following TDABC guidelines as follows [32]:
To account for the sub-departments mentioned previously, we expand this formula to recognize different resource needs within a single activity as follows:
where CCRn is the capacity cost rate of resource pool n, and where time required can be unique to a resource, and can depend on a cost predictor k. A care path consists of multiple such activities or processes. Cost predictors can equal 1 in case no predictor is present and variation is negligible. The resulting CCRs, and their components, are provided in appendix D. The resulting model was programmed into an interactive tool in Microsoft ® Office Excel ® due to its universal availability in clinical settings, and with data safety in mind, as the tool does not require an internet connection or data transfer.
Finally, we applied process mining using Fluxicon Disco to discover patient trajectories in 10 years of clinical data from this clinic [43, 44], based on the treatment categories identified in the TDABC analysis (i.e., treatment types within DRGs that features significantly different costs, such as sub-categories of IVF). For example, within IVF-ICSI treatments, a small IVF-ICSI treatment consumes significantly fewer resources than a large combination cycle (IVF-Combi). These categories were thus incorporated in the process mining analysis, rather than relying aggregate treatment labels alone. The full patient sample (n = 6.822) was restricted to patients that started and ended their treatment journey between 1/1/2014 and 1/1/2023 and that completed at least one cycle of care (to exclude patients only seeking a second opinion, or those still undergoing care today), resulting in a consolidated sample of 3.335 female patients covering 13.203 treatment cycles, and data on their partners (or donors).
Results
The treatment options available are summarized in the process map in Fig. 1. Patients can repeatedly cycle through, and switch between, four alternative treatment options as described in Sect. "Setting". These include two kinds of ovulation induction (OI), in-vitro fertilization (IVF), or intra-uterine insemination (IUI). In-vitro fertilization (IVF) involves four distinct phases: stimulation, follicle aspiration, fertilization, and embryo transfer. These generate frozen embryos, which are used in subsequent frozen embryo transfer (FET) cycles during which a frozen embryo is thawed and placed into the uterus. Decisions made during IVF impact the processes used during FET cycles; for example, if embryos are frozen using cryopreservation m methods, they must be thawed using the same medical protocol. One cycle of IVF can involve many FET attempts, each lasting one month, depending on the number of embryos generated and frozen during IVF. Patients can repeat treatments or switch to different treatments after each monthly cycle. The distinction between IVF and ICSI comes from the technology used to complete the fertilization phase of IVF. An IVF cycle thus has four options that differ in resource consumption: IVF, IVF-ICSI, IVF-Combi. IVF-Combi can be disaggregated down further into intentional IVF-Combi cycles and rescue-ICSI cycles. In an IVF-Combi cycle half of all oocytes are fertilized with IVF, and half with ICSI. In case of a rescue-ICSI cycle, oocytes are fertilized with the ICSI technology if no oocytes are fertilized through IVF earlier that same day. This means that they require significantly more resources, but are highly valuable, as patients would otherwise have been guaranteed a poor outcome (no chance of pregnancy) and subsequent IVF or ICSI treatments. We provide a summary of the relevant European clinical guidelines in appendix A. The medical metro line, which depicts all individual activities costed per treatment type, is provided in appendix B. Appendix B covers all processes shown in Fig. 1, and an example is provided later in Fig. 4.
Macro and meso-level process map depicting the four possible treatment types. Note: ICSI, intracytoplasmic sperm injection. Filled long rectangles indicate processes, which are split into sub-processes. A failed cycle can be followed by another cycle (same or a different treatment). If embryos are frozen during IVF, thawing can be planned and initiated the following cycle or later (FET). FET is recognized as a sub-process of IVF but involves a new cycle that resembles IVF but uses thawed embryos
Observations, cost predictors (k) and capacity cost rates (CCRs)
Observations related to the IVF pathway exhibited the longest durations and greatest variation; whilst an average IVF cycle required 313 min of lab staff time, ICSI and IVF-ICSI required 386 and 445 min, respectively. We identified six core cost predictors. These are clinical decisions or patient-level factors that lead to higher resource utilization per patient:
-
(1)
The type of semen wash technique required,
-
(2)
The number of predicted oocytes based on ultrasounds,
-
(3)
The realized number of oocytes retrieved after a follicular aspiration,
-
(4)
The number of consultations and ultrasounds required,
-
(5)
The number of embryos fertilized using IVF, IVF-ICSI, rescue-ICSI, or ICSI, and.
-
(6)
The type of technique used to freeze (during IVF) and thaw (during FET) embryos.
In total, 13 CCRs were determined to allocate costs, and these reflect the unique resource requirements of all care delivered (e.g., laboratory staff, laboratory equipment specific to IVF, ICSI, etc.). These 13 CCRs are minimally necessary to respect TDABC’s principle of homogeneity [32], which specifies that CCRs must be constructed such that no costs are allocated to objects that do not consume them, and that departmental CCRs are only applicable if each service delivered by the department uses the same mix of resources. However, as each treatment delivered by the fertility clinic uses a different mix of resources (e.g., ICSI treatments use different resources than IVF, and OI treatments use no laboratory resources at all, and IUI treatments use a different sub-department of the laboratory than IVF and ICSI) a single CCR is inadequate, and both the laboratory and clinical areas of the clinic needed to be split into separate cost rates i.e. sub-departments. The durations and cost predictors determined using observations are available in appendix C. The CCRs are described in appendix D. The cost equations, which multiply the CCRs with the duration of care processes, are provided in appendix E in the form of an interactive tool which can either be used verbatim or as a template. Patient-level variation is incorporated through cost predictors; by entering the parameters of the 6 cost predictors identified above, the equations produce cost estimates that reflect them, rather than assuming static cost objects per treatment type like DRGs do [45]. In this way, patients that require more materials and HCP’s time, due to e.g. a large cycle size, are allocated more costs than those requiring fewer materials and/or time.
Average total costs of care per treatment cycle (within DRGs)
Table 2 displays the total costs per treatment type determined using TDABC, and a percentage breakdown of the cost sources per resource (CCR). We find that an average initial fertility assessment (IFA), excluding extensive diagnostics such as an operation, costs €504 to deliver in total. An average natural, unstimulated cycle of IUI costs €518, and a stimulated cycle €845. One cycle of OI using Clomid CC or Letrozole as a stimulation agent costs €221, consisting primarily of consultations. Using FSH stimulation raises that amount to a total of €963 due to the additional monitoring appointments and medications required. One average cycle of IVF costs a total of €2.610 to deliver, with IVF lab staff (25%) and lab material and equipment (15%) representing the greatest source of costs after medications. An average ICSI cycle costs €3.005, and a combination cycle €3.193. Offering both types of fertilization in one combination cycle (IVF-Combi) requires separate preparation for and administration of each half of the oocytes retrieved, resulting in the highest workload in the lab, generating higher costs. Further, this is only offered to patients with more than 10 oocytes in a cycle, resulting in a higher-than-average volume of patient material to manage in the lab for these specific cycles. A FET costs between €922 and €1.036 per cycle.
The analysis underscores a tradeoff: higher costs are incurred with increased volumes of patient materials processed in the laboratory during IVF cycles. However, this added workload is exceptionally valuable to patients and the healthcare system as it raises the likelihood of reaching pregnancy, reducing the necessity for additional cycles of care later [1, 46], raising the likelihood of timely pregnancies. This is because, following IVF or ICSI, patients can undergo FET treatments which are less invasive and much lower in costs. So, delivering costly high-volume IVF-cycles is valuable overall, both to patients and the healthcare system, but is currently very costly to clinics. Table 3 illustrates the impact of cycle size on costs incurred, and how frequently each type occurs in our sample as percentages.
More ICSI and combination cycles are administered compared to IVF-only cycles, and these cycles tend to be of medium or large size. While the cost of IVF-only cycles ranges from €2.479 (32%) to €2.825 (32%), ICSI cycles range from €2.740 (22%) to €4.089 (42%), and combination cycles range from €3.010 (35%) to €3.617 (65%). However, under the current DRG as per 2023, all cycles are reimbursed at a fixed rate of €2.955 for IVF and €3.064 for ICSI and combination cycles, regardless of their size [28]. This reimbursement amount falls short of the estimated costs presented here, which generates losses for clinics for high-volume cases (which are most common). For example, 42% of ICSI cases were large, costing €4.089 to deliver yet generating DRGs of €3.064 (or less in prior years), which is a discrepancy of €1.025 or a shortcoming of 33%. These cost estimates are conservative, under ideal conditions, and only incorporate resources used; they exclude e.g., spare equipment like spare microscopes maintained purely to ensure services levels, and they exclude repeated activities e.g., repeated embryo thaws (which are common in practice).
Total costs of care per patient journey or trajectory (across DRGs)
As patient journeys consist of many rounds of care, understanding patient-level costs and the impact of treatment choices requires an analysis of patient trajectories. Using the costing model developed, costs can be estimated using sample averages (as shown in Tables 1 and 2), or alternatively at the patient level using individual input parameters per patient. We constructed an event log of the patient sample, with each event corresponding to one process costed with TDABC and simulated the total costs of care per patient and pregnancy pathway for the entire sample. The patient sample is summarized in Table 4.
On average, pathways from first consult to end (pregnancy, birth, or end of treatment) took 25,5 months at mean cost of €6.329 (3.335 patients). This includes cases of multiple pregnancies, with or without births, and cases that never once reach pregnancy (shown in Fig. 2 and Table 4). Consequently, the costs of these pathways ranged significantly, from €221 to €36.976, and their duration varied from 30 days to 8,59 years.
Alternatively, when considering each pregnancy achieved or strived for as a separate pathway, and thus subsequent attempts at pregnancy by the same patient or couple as a separate trajectory, mean costs were €5.037 with a mean duration of 20,3 months, and with costs ranging from €162 to €30.074. Of these 4.190 trajectories relating to the 3.335 patients, 1.411 resulted in live births (36,8%), which is above average [5]. Notably, high resource utilization was most common among those patients who never reached a single pregnancy, whilst patients who gave birth twice or more required significantly fewer resources and fewer cycles of care in total, shown in Fig. 2.
We present the most prevalent patient pathways for the entire sample, per patient, in Fig. 3. Each treatment box contains the total frequency per treatment, and the maximum number of repetitions per case in brackets. The most common treatment type is IUI, followed by FET cycles after IVF, which both feature many repetitions. Given the prior cost results and given that patients frequently repeat IVF and FET cycles, it can be concluded that significant cost reductions can be gained from avoiding failed cycles of IVF, IVF-ICSI, or combination cycles, and from reducing the per-cycle costs of each individual IVF and FET, as these are frequently repeated (up to 17 times by a single patient in case of FET). Choices made, and outcomes achieved, during IVF treatments causally determine costs incurred during FET cycles; for instance, how many embryos are generated and frozen, and how they are frozen, determines the number of FET cycles that are possible and their costs.
Overview of pathways after diagnostics (4.190 trajectories from first consultation to pregnancy). Note: FET, Frozen embryo transfer; ICSI: intracytoplasmic sperm injection; IUI: intra-uterine insemination; IVF: in-vitro fertilization; Expectative: skipped or cancelled cycle due to e.g. cycle failure. Each rectangle contains the total frequency of treatment rounds, and the maximum repetitions per patient per treatment type in brackets. Arrows depict the most dominant patient flows, including frequency. Max. repetitions are given in brackets
Cost variation and savings within DRGs, and across patient pathways
Given the findings presented in the prior sections, we evaluate two methods that reduce burden on the laboratory phases of IVF: (1) vitrification, which is a new means of embryo freezing and thawing (refer to Fig. 1 FET), and (2) artificial embryo selection using time-lapse imaging during the fertilization phase (refer to Fig. 1 IVF). These methods reduce costs within treatment/DRG categories and have significant economic impact across patient trajectories from initial consultation to pregnancy; such dependencies between treatments must be accounted for when calculating opportunity costs for economic analyses [2, 4, 6, 36], but our results indicate that they are not currently reflected in DRGs, which may misalign incentives [31].
First, our results show that quick freeze vitrification during IVF reduces the costs of that IVF cycle [47], and costs of all subsequent FET cycles, and positively impacts the chance of pregnancy. The difference stems from the fact that vitrification is quicker to perform, both whilst freezing (during IVF cycle) and thawing (during FET cycle) as shown in appendix C. Because thawing after quick freeze vitrification significantly reduces the workload for clinicians (26 vs. 50 min), more embryos can be thawed on the day of the procedure, and these embryos are less likely to degenerate. This is extremely valuable, as the embryo transfer must be cancelled if no viable embryo is available at the time of the procedure (this implies the entire month-long treatment must be repeated). Further, embryos thawed with vitrification can be evaluated more quickly, which has significantly reduced cancellation rates in comparison to cryopreservation methods. This makes it a significant and value-adding clinical choice, as it improves both costs and success chances during subsequent treatments. On the other hand, embryos thawed with cryopreservation need continued monitoring over 30 min-3 h to determine if they are viable or not, which significantly increases work; prior to this assessment, no further embryos can be thawed. This evaluation delay can cause a treatment cycle failure if the thawed embryo is evaluated to be unusable, but insufficient time is left to thaw and evaluate another one. These dependencies, and the critical role of embryo availability, are depicted in Fig. 4 column 9–10. Cycles that fail towards the end of the cycle, on the day of the embryo transfer due to embryo unavailability, are extremely costly to deliver and hold no patient value; without an embryo transfer there is zero chance of a positive outcome (pregnancy), and all of the resources and costs relating to columns 1–11 in Fig. 4 have already been incurred. These represent 80% of total treatment delivery costs shown in Table 2.
Metro line showing all steps for FET delivery, based on observations and real-world data according to European standards. Red paths signify poor outcomes (e.g., repeated cycles, no pregnancy). Circles represent activities; stars denote shared decision-making points, diamonds indicate alternative routes, white circles denote tasks performed by healthcare providers without patient presence, and filled circles represent activities with patient involvement
Whilst freezing with vitrification only minorly impacts the costs within the IVF cycle (€13 savings), it significantly reduces costs of subsequent FET cycles due to more efficient processing (€98 savings per vitrification thaw, due to quicker processing time). Thus, if a patient’s embryos are frozen using vitrification during IVF, this benefits all subsequent FET cycles and relieves overall workload in the laboratory, which is preferable to embryologists and laboratory technicians. In our sample, patients that underwent IVF required up to 8 rounds of IVF (IVF, IVF-ICSI, or IVF-Combi), and up to 17 rounds of FET (Fig. 3). In an average case, vitrification vs. usual care thus saves €322 per patient pathway across all FETs, and in extreme cases (17 repetitions) up to €1.998 per patient pathway, at superior medical performance [47]. This superior performance further reduces embryo degeneration chances within the IVF treatment cycle [47], which avoids additional treatment rounds (€940—€4.089 savings per additional FET or IVF avoided, see Tables 2 and 3). Improving time-to-pregnancy by reducing the number of treatments required is highly valuable to patients, as treatments are painful and invasive. It is also valuable to the healthcare system, as it would reduce waiting times, which in turn benefits other patients because success chances decrease with patient age. As about 50% of all Dutch cycles are FET cycles (Table 1), the annual savings of using vitrification instead of cryopreservation amount to €1.311.396 (€98 × 13.382 average annual FET treatments), whilst improving laboratory workflow, workload, and value to patients by reducing the chances of treatment failures. Given that 225.744 FET cycles are delivered on average in Europe, choosing vitrification may also reduce workload or costs across Europe.
Secondly, algorithmic embryo evaluation reduces time spent by HCPs and improves medical performance [48,49,50], which is consistent with our observations (appendix C). High utilizers of care are those patients that undergo multiple large cycles of IVF (either IVF, IVF-ICSI, IVF-Combi) and subsequent FETs, which can be repeated until no embryos remain. Avoiding just one additional cycle thus saves between €940 and €4.089 in costs. These efforts are being combined with training in a so-called ‘rescue-ICSI’ wherein oocytes not fertilized with IVF are treated with ICSI within 24 h of failed fertilization [51], to attempt to avoid a failed cycle by fertilizing the oocytes manually through injection using ICSI techniques. This provides patients, who would have ordinarily had a failed cycle, additional chances of pregnancy in that same treatment cycle, and is therefore extremely valuable because it reduces total treatment duration and costs per patient. Further, as patients must undergo painful and/or invasive hormonal stimulation in the first weeks of IVF to overstimulate oocyte production (see Fig. 1 and appendix B), offering an additional chance of fertilization per stimulation phase would reduce patient discomfort. The cost of the rescue-ICSI cycle is comparable to large IVF-Combi cycles, as rescue-ICSI cycles require the same activities and utilize the same resources (it also involves processing oocytes twice using first the IVF technique and then ICSI like in the combination cycle). However, delivering a rescue-ICSI cycle thus exceeds the allotted DRG of €3.064, but if successful avoids an additional IVF cycle (thus saving between €2.479-€4.089). Thus, if a clinic chooses to invest in this technique and intervene in a failed IVF cycle using rescue-ICSI, the clinic incurs financial losses. However, if this rescue-ICSI is successful in either causing pregnancy or in generating frozen embryos that can be used in subsequent FET cycles (which are less costly than IVF or ICSI cycles), this rescue-ICSI procedure will have improved patient comfort, reduced the total costs of care across the patients’ treatment pathway, and will have reduced resource wastage by avoiding one cycle of IVF or IVF-ICSI.
Our analysis revealed further opportunities for value improvements. Due to the high costs associated with all types of IVF, value could be increased and workload decreased by improving the flow of preparatory work in the laboratory through e.g., automated dish labelling or bar coding. Another factor would be to improve cycle size estimation techniques, as the preparatory work is done based on estimated follicle counts. To illustrate, the preparatory work one day prior to the follicular aspiration costs on average €143 and €346 for IVF and IVF-ICSI, respectively, which is greater for high-volume cases (refer to Table 3). These opportunity costs associated with vitrification, rescue-ICSSI, and AI embryo selection cannot currently be determined by clinicians using DRGs, because DRGs don’t account for which technology is used, how large a cycle is, or how decisions made in one treatment impacts costs in later treatments for the same patient.
Discussion and conclusion
We conducted a comprehensive cost analysis of entire patient pathways from initial consultation to pregnancy to examine cost variations and determine the minimal costs of delivering fertility treatments under European standards. Because treatments are repetitive and inter-dependent, and laboratory phases of care are most costly, our results show that clinical decisions in one treatment impact costs and value in subsequent treatments. Our analysis demonstrates the importance of granular cost evaluations for decision-making in settings where aggregate DRGs alone don’t enable such comparisons. We contribute to the emergent literature on TDABC, to literature on the economics of subfertility, and to policymakers hoping to address rising costs of subfertility. By providing granular costing infrastructure using real-world data, and by evaluating emerging technologies vs. usual care, we also offer actionable tools to healthcare providers to implement value-based strategies for personalized fertility care.
First, our study contributes to the ongoing discussion of the applicability of DRGs for economic analyses [2, 12, 15, 37, 40, 52, 53], as we directly examine their utility and relevance to decision-making and analysis in the European fertility care setting. Our approach (TDABC using participant observations) has generated insights into cost variation within DRG/treatment categories, which has enabled both managerial decision-making and opportunity cost explorations within treatment categories at the clinic [14], which was not possible using aggregate DRGs [2]. Our findings suggest that IVF and ICSI reimbursements should be updated to reflect the current high practice variety in treatments present in Europe, as the DRG categories hide the significant resource requirement differences between sub-categories – for example, costs vary by 60% (€2.585-€4.089) in the case of ICSI treatments, and large ICSI cycles are most common (41% of our sample), but drastically exceed their DRG (€4.089 costs vs. €3.064 reimbursement, 33% shortcoming to cover costs estimated under ideal conditions). We thus illustrate that implementing TDABC for complex care at scale is feasible, advantageous, and can inform economic analyses, which complements recent work from non-complex care settings like surgical interventions [18, 33, 54, 55]. In this study, we focused on cost variation, and the impact of emerging technologies on costs and outcomes. Future research should explore determinants of total patient journey costs and outcomes, e.g. in relation to multimorbid diagnoses like endometriosis or ovulation disorder, or patient-level characteristics like age. This could shed light on the causes of variation in the cost predictors we identified (e.g. number of consultations needed). Additionally, whilst we compared IVF costs with DRGs, future work could compare total patient journey costs and DRGs, as the demand for IVF specifically is increasing. This would shed light on whether clinics are facing financial struggles due to increasing IVF treatment volume and cycle size increases.
Secondly, we contribute to the health economics literature on fertility care [19, 56], which has featured recent and explicit calls for granular cost evaluations, given the increasing practice variation within treatments [16]. This need is accentuated by escalating subfertility prevalence, treatment demands, and the desire to deliver patient-centered treatments tailored to individuals’ needs (i.e. personalized care) [19, 22, 26, 57, 58]. In patient pathways involving IVF or IVF-ICSI, our analysis reveals notable cost discrepancies among treatment modalities, patient pathways, and technologies, resulting in diverse costs and outcomes not reflected by broad treatment labels. Notably, current Dutch DRGs fail to promote per-patient cost reductions due to inter-cycle dependencies (e.g. choices made during IVF impact the costs of FETs) and inadequate coverage for interventions like rescue-ICSIs, leading to organizational financial losses for clinics despite long-term cost savings per patient from the perspective of healthcare systems. We problematize this because clinics need to be able to invest in new technologies that improve costs and outcomes per patient, and because the demand for IVF is rising as subfertility rates rise. Delivering one large IVF cycle with a rescue-ICSI procedure would be favorable compared to two separate cycles, but this results in organizational losses to clinics, because this essentially requires two treatments in one cycle that is currently only reimbursed one DRG.
While reaffirming previous research on IVF costliness compared to OI and IUI [5, 7, 8, 17, 59], our study identifies causal sources of cost variation at treatment, process, and patient levels, highlighting how clinical choices causally relate to cost differences over time. Our findings suggest a structural gap in the current reimbursement system, which assumes static resource consumption per treatment [5, 6, 17, 60], and which fails to incentivize treatments like IVF-Combi or rescue-ICSI despite their value to patients [51]. Providing these treatments is very valuable to patients and society but generates short-term financial losses for clinics, which remain economically invisible when relying on aggregate DRGs alone. This finding may explain part of the significant variation in total fees documented in the UK [5], US [6] and globally [7, 8], as these studies have relied on DRGs and thus assumed static laboratory burden per treatment type. Given that cost information accuracy is crucial for decision-making [40, 61], our results highlight the need for granular cost estimates that reflect patient-level (e.g., oocytes and embryo volumes) and treatment-level (IVF, IVF-ICSI, rescue-ICSI, IVF-Combination, FET with vitrification vs. FET with cryopreservation) cost variation for the purpose of local organizational decision-making and economic analyses or policies. Economic analyses rely on differential costs that accurately reflect the resource consumption—thus, granularity is necessary within IVF and ICSI to reflect these significant differences [2].
When considering entire patient pathways, technologies that enable more efficient preparation and work in the laboratory (e.g., vitrification) have a significant impact on per-patient costs, even if per-cycle cost reductions seem limited, due to the number of repetitions of treatments. Whilst prior research emphasized the need to reduce medication costs or monitoring costs in IVF [6, 17, 26, 62], our findings suggest that future work should also consider reducing laboratory burden, specifically in high-volume cases that are increasingly common (e.g., 64,9% of IVF-Combi are large, and 41% of IVF-ICSI are large). Because annual FET cycle numbers are rising in Europe and globally, with e.g., the US predicted to exceed 1 m annual FET cycles [30, 57], clinics are encouraged to adopt vitrification to reduce the total economic burden of subsequent FET cycles.
Thirdly, our study contributes to the recent and active debate regarding the feasibility and utility of TDABC in complex care settings [18, 35, 55], and the associated infrastructure requirements of routine patient-level cost estimations to implement VBHC [5, 11, 14, 15, 17, 26, 63]. This is particularly relevant in settings such as IVF, which feature constantly developing medical technologies, all of which change treatment protocols and thus result in cost differences within treatment categories [64]. Our study, and the tool we have developed (appendix E) demonstrates the feasibility and utility of combining TDABC with PM for routine cost estimation in complex care settings, addressing current calls for the implementation of patient-centered cost measurement [18, 35, 52, 55]. Specifically, we demonstrate that TDABC can be used to create tailored costing systems that allocate direct and indirect costs of care to patient trajectories, that support decision-making through comparisons of alternatives that are not reflected in prices [61]. As care delivery becomes increasingly personalized, and as the medical science of embryology continues to discover alternative laboratory techniques, such comparisons are relevant to improving care access, sustainability, and value. This addresses prior concerns regarding the feasibility of TDABC implementation in complex care [11, 52, 54], as we demonstrate how it can be incorporated with real-world clinical data using PM to capture entire patient pathways. Our study further highlights the need for transmural data collection regarding care activities (rather than medical outcomes) and organizational accounting data (rather than reimbursements) [2, 9].
Our study also offers practical insights to practitioners implementing TDABC. Whilst some studies suggest that time estimates are sufficient for TDABC analyses [18, 32, 65], our experience in complex care has been different. Specifically, we relied on participant observations to derive duration measurements, as staff were unable to confidently estimate durations for procedures that varied due to the personalization of care. Duration measurement limits estimation error and reduces chances of model manipulation [66, 67]. Because observational measures were key to identifying the variation and cost predictors, we encourage future work to incorporate duration measures as best practice, which builds on prior best practice reports [18, 68]. In addition to this, future research using this methodology should publish the choices made in such analyses transparently (i.e., activities costed, CCRs constructed, time estimates used) as cost accounting methodologies like TDABC cannot be standardized [12, 36,37,38, 40, 63, 69]. Our work underscores the importance of CCR granularity, as CCR granularity determines the granularity of the results generated [39]. Specifically, exploring within-treatment variation requires that CCRs are more granular than DRG or treatment categories themselves, and/or that duration measurements vary within DRG categories and ideally depend on patient-level factors (such as in our case cycle volume, number of consultations, etc.). One limitation of TDABC generally and our study specifically is that this method does not allocate fixed overheads when they are shared with other departments [40]. To limit the impact of this shortcoming, we conducted this study at a clinic not physically embedded in a hospital. This means that minor fixed overheads (e.g. website maintenance) were excluded from this analysis. A second limitation of this study relates to generalizability, as our study is generalizable to other clinics following European guidelines but will require updates in future as treatment protocols evolve, new laboratory technologies emerge, and as the cost of materials and labor change over time and between locations. The strength of the method lies in its ability to capture such variation.
In conclusion, this cost analysis has revealed significant cost variation within treatment categories for IVF and ICSI treatments, which add up across patient journeys when considering entire trajectories from initial consultation to pregnancy or birth. Costs within the various sub-categories of IVF are significantly influenced by the volume of patient material handled in the lab, which varies per patient and laboratory method. Reducing the number of unsuccessful cycles of care is the most meaningful way to realize value-based fertility care, which current aggregate DRGs may not incentivize or make visible. IVF related DRGs could be improved by introducing granularity through the categories identified throughout this study. Care providers are encouraged to use the costing tool developed in this study (appendix E), by inputting their own annual cost data and duration measures to estimate costs for patient pathways, and treatment cycles. This would allow for routine (e.g., quarterly) updating of cost estimates in line with the rapid development of medical science and technology in embryology, and transparent publication of granular cost estimates could inform appropriate and timely reimbursement policies and economic analyses.
Data availability
All data generated is available in the supplementary appendix. De-identified patient pathway data are available on request from the corresponding author.
References
Keller, E., Chambers, G.M.: Valuing infertility treatment: Why QALYs are inadequate, and an alternative approach to cost-effectiveness thresholds. Front. Med. Technol. 4, 1053719 (2022). https://doi.org/10.3389/fmedt.2022.1053719
Špacírová, Z., Epstein, D., Espín, J.: Are costs derived from diagnosis-related groups suitable for use in economic evaluations? A comparison across nine European countries in the European Healthcare and Social Cost Database. Eur. J. Health Econ. 23, 1563–1575 (2022). https://doi.org/10.1007/s10198-022-01444-y
Busse, R., Geissler, A., Quentin, W., Wiley, M.M.: Diagnosis-Related Groups in Europe: moving towards transparency, efficiency and quality in hospitals. Open University Press, Buckingham, England (2011)
Pöhlmann, J., Norrbacka, K., Boye, K.S., Valentine, W.J., Sapin, H.: Costs and where to find them: identifying unit costs for health economic evaluations of diabetes in France, Germany and Italy. Eur. J. Health Econ. 21, 1179–1196 (2020). https://doi.org/10.1007/s10198-020-01229-1
Bahadur, G., Homburg, R., Bosmans, J.E., Huirne, J.A.F., Hinstridge, P., Jayaprakasan, K., Racich, P., Alam, R., Karapanos, I., Illahibuccus, A., Al-Habib, A., Jauniaux, E.: Observational retrospective study of UK national success, risks and costs for 319,105 IVF/ICSI and 30,669 IUI treatment cycles. BMJ Open 10, e034566 (2020). https://doi.org/10.1136/bmjopen-2019-034566
Katz, P., Showstack, J., Smith, J.F., Nachtigall, R.D., Millstein, S.G., Wing, H., Eisenberg, M.L., Pasch, L.A., Croughan, M.S., Adler, N.: Costs of infertility treatment: results from an 18-month prospective cohort study. Fertil. Steril. 95, 915–921 (2011). https://doi.org/10.1016/j.fertnstert.2010.11.026
Chambers, G.M., Adamson, G.D., Eijkemans, M.J.C.: Acceptable cost for the patient and society. Fertil. Steril. 100, 319–327 (2013). https://doi.org/10.1016/j.fertnstert.2013.06.017
Connolly, M.P., Hoorens, S., Chambers, G.M.: ESHRE reproduction and society task force: the costs and consequences of assisted reproductive technology: an economic perspective. Hum. Reprod. Update 16, 603–613 (2010). https://doi.org/10.1093/humupd/dmq013
Llewellyn, S., Northcott, D.: The average hospital. Account. Organ. Soc. 30, 555–583 (2005). https://doi.org/10.1016/j.aos.2004.05.005
Lindgren, P., Althin, R.: Something borrowed, something new: measuring hospital performance in the context of value based health care. Eur. J. Health Econ. 22, 851–854 (2021). https://doi.org/10.1007/s10198-020-01209-5
Cossio-Gil, Y., Omara, M., Watson, C., Casey, J., Chakhunashvili, A., Gutiérrez-San Miguel, M., Kahlem, P., Keuchkerian, S., Kirchberger, V., Luce-Garnier, V., Michiels, D., Moro, M., Philipp-Jaschek, B., Sancini, S., Hazelzet, J., Stamm, T.: The roadmap for implementing value-based healthcare in European university hospitals-consensus report and recommendations. Value Health. 25, 1148–1156 (2022). https://doi.org/10.1016/j.jval.2021.11.1355
Tan, S.S., Serdén, L., Geissler, A., van Ineveld, M., Redekop, K., Heurgren, M.: DRGs and cost accounting: which is driving which? In: Busse, R., Geissler, A., and Quentin, W. (eds.) Diagnosis-Related Groups In Europe: Moving Towards Transparency, Efficiency And Quality In Hospitals. pp. 59–74. European 1574 Z. Špacírová et al. 1 3 Observatory on Health Systems and Policies Series, Maidenhead, Open University Press McGraw-Hill, Berkshire (2011) (2011)
Preston, A.M.: The birth of clinical accounting: a study of the emergence and transformations of discourses on costs and practices of accounting in U.S. hospitals. Account. Organ. Soc. 17, 63–100 (1992). https://doi.org/10.1016/0361-3682(92)90036-R
Ederhof, M., Ginsburg, P.B.: “Meaningful use” of cost-measurement systems - incentives for health care providers. N. Engl. J. Med. 381, 4–6 (2019). https://doi.org/10.1056/NEJMp1900329
Ederhof, M., Ginsburg, P.B.: Improving hospital incentives with better cost data. N. Engl. J. Med. 376, 1010–1011 (2017). https://doi.org/10.1056/NEJMp1613181
Leusder, M., van Elten, H.J., Ahaus, K., Hilders, C.G.J.M., van Santbrink, E.J.P.: Protocol for improving the costs and outcomes of assistive reproductive technology fertility care pathways: a study using cost measurement and process mining. BMJ Open 13, e067792 (2023). https://doi.org/10.1136/bmjopen-2022-067792
Bouwmans, C.A.M., Lintsen, B.M.E., Eijkemans, M.J.C., Habbema, J.D.F., Braat, D.D.M., Hakkaart, L.: A detailed cost analysis of in vitro fertilization and intracytoplasmic sperm injection treatment. Fertil. Steril. 89, 331–341 (2008). https://doi.org/10.1016/j.fertnstert.2007.03.003
Leusder, M., Porte, P., Ahaus, K., van Elten, H.: Cost measurement in value-based healthcare: a systematic review. BMJ Open 12, e066568 (2022). https://doi.org/10.1136/bmjopen-2022-066568
Nargund, G., Datta, A.K.: Maximizing live birth rates cannot be the only key performance indicator of IVF. Reprod. Biomed. Online 44, 587–589 (2022). https://doi.org/10.1016/j.rbmo.2021.11.011
Chambers, G.M., Dyer, S., Zegers-Hochschild, F., de Mouzon, J., Ishihara, O., Banker, M., Mansour, R., Kupka, M.S., Adamson, G.D.: International committee for monitoring assisted reproductive technologies world report: assisted reproductive technology, 2014. Hum. Reprod. 36, 2921–2934 (2021). https://doi.org/10.1093/humrep/deab198
Sumant, O., Joshi, K.: Fertility services market by procedure (IVF with ICSI, IUI, IVF without ICSI, surrogacy, and others) and service (Fresh non-donor, frozen non-donor, egg and embryo banking, fresh donor, and frozen donor): global opportunity analysis and industry forecast. (2019)
WHO: Infertility prevalence estimates, 1990–2021. WHO (2023)
WHO: WHO fact sheet on infertility. Glob. Reprod. Health. 6, e52 (2021). https://doi.org/10.1097/grh.0000000000000052
ESHRE: Factsheets and infographics, https://www.eshre.eu/Europe/Factsheets-and-infographics, Accessed December 6, 2023
ASRM: Quick Facts About Infertility, https://www.reproductivefacts.org/faqs/quick-facts-about-infertility/, Accessed December 6, 2023
Gerris, J.M.R., Fauser, B.C.J.M.: Home monitoring of ovarian stimulation: an important step towards more patient-centred IVF. Reprod. Biomed. Online 41, 971–974 (2020). https://doi.org/10.1016/j.rbmo.2020.10.014
Rienzi, L., Fauser, B.: Future challenges for clinical embryologists. Reprod. Biomed. Online 43, 973–975 (2021). https://doi.org/10.1016/j.rbmo.2021.10.001
NZa: Prestatie- en tariefbeschikking medisch-specialistische zorg TB/REG-22613–02 - Nederlandse Zorgautoriteit, https://puc.overheid.nl/nza/doc/PUC_652110_22/
NVOG: Landelijke IVF-cijfers 2020, Stichting LIR. Nederlandse Vereniging voor Obstetrie & Gynaecologie (2022), https://www.degynaecoloog.nl/wp-content/uploads/2022/02/IVFlandelijk2020.pdf. Accessed December 6, 2023
ESHRE: ART in Europe, 2019: results generated from European registries by ESHRE. Hum. Reprod. 38, 2321 (2023). https://doi.org/10.1093/humrep/dead197
Gajadien, C.S., Dohmen, P.J.G., Eijkenaar, F., Schut, F.T., van Raaij, E.M., Heijink, R.: Financial risk allocation and provider incentives in hospital-insurer contracts in The Netherlands. Eur. J. Health Econ. 24, 125–138 (2023). https://doi.org/10.1007/s10198-022-01459-5
Kaplan, Anderson, S.: Time-driven activity-based costing: A simpler and more powerful path to higher profits. Harvard Business Press, Boston, MA (2007)
Keel, G., Muhammad, R., Savage, C., Spaak, J., Gonzalez, I., Lindgren, P., Guttmann, C., Mazzocato, P.: Time-driven activity-based costing for patients with multiple chronic conditions: a mixed-method study to cost care in a multidisciplinary and integrated care delivery centre at a university-affiliated tertiary teaching hospital in Stockholm, Sweden. BMJ Open 10, e032573 (2020). https://doi.org/10.1136/bmjopen-2019-032573
Berthelot, S., Mallet, M., Blais, S., Moore, L., Guertin, J.R., Boulet, J., Boilard, C., Fortier, C., Huard, B., Mokhtari, A., Lesage, A., Lévesque, É., Baril, L., Olivier, P., Vachon, K., Yip, O., Bouchard, M., Simonyan, D., Létourneau, M., Pineault, A., Vézo, A., Stelfox, H.T.: Adaptation of time-driven activity-based costing to the evaluation of the efficiency of ambulatory care provided in the emergency department. J. Am. Coll. Emerg. Phys. Open. 3, e12778 (2022). https://doi.org/10.1002/emp2.12778
Tan, S.S., Bakker, J., Hoogendoorn, M.E., Kapila, A., Martin, J., Pezzi, A., Pittoni, G., Spronk, P.E., Welte, R., Hakkaart-van Roijen, L.: Direct cost analysis of intensive care unit stay in four European countries: applying a standardized costing methodology. Value Health. 15, 81–86 (2012). https://doi.org/10.1016/j.jval.2011.09.007
Tan, S.S., Geissler, A., Serdén, L., Heurgren, M., van Ineveld, B.M., Redekop, W.K., Hakkaart-van Roijen, L.: EuroDRG group: DRG systems in Europe: variations in cost accounting systems among 12 countries. Eur. J. Public Health 24, 1023–1028 (2014). https://doi.org/10.1093/eurpub/cku025
Malmmose, M., Lydersen, J.P.: From centralized DRG costing to decentralized TDABC-assessing the feasibility of hospital cost accounting for decision-making in Denmark. BMC Health Serv. Res. 21, 835 (2021). https://doi.org/10.1186/s12913-021-06807-4
Clark, J.M.: Studies in the Economics of Overhead Costs. University of Chicago Press (1923)
Demeere, N., Stouthuysen, K., Roodhooft, F.: Time-driven activity-based costing in an outpatient clinic environment: development, relevance and managerial impact. Health Policy 92, 296–304 (2009). https://doi.org/10.1016/j.healthpol.2009.05.003
Špacírová, Z., Epstein, D., García-Mochón, L., Rovira, J., de Labry, O., Lima, A., Espín, J.: A general framework for classifying costing methods for economic evaluation of health care. Eur. J. Health Econ. 21, 529–542 (2020). https://doi.org/10.1007/s10198-019-01157-9
Panteon: Samen beslissen in de zorg ondersteunen met service design, https://metromapping.org/, Accessed December 6, 2023
ESHRE: ESHRE Guidelines, Consensus Documents and Recommendations, https://www.eshre.eu/Guidelines-and-Legal, Accessed December 6, 2023
Rismanchian, F., Kassani, S.H., Shavarani, S.M., Lee, Y.H.: A data-driven approach to support the understanding and improvement of patients’ journeys: a case study using electronic health records of an emergency department. Value Health. 26, 18–27 (2023). https://doi.org/10.1016/j.jval.2022.04.002
De Roock, E., Martin, N.: Process mining in healthcare - An updated perspective on the state of the art. J. Biomed. Inform. 127, 103995 (2022). https://doi.org/10.1016/j.jbi.2022.103995
Llewellyn, S., Chambers, N., Ellwood, S., Begkos, C., Wood, C.: Patient-level information and costing systems (PLICSs): a mixed-methods study of current practice and future potential for the NHS health economy. NIHR Journals Library, Southampton (UK) (2016)
Bahadur, G., Homburg, R., Jayaprakasan, K., Raperport, C.J., Huirne, J.A.F., Acharya, S., Racich, P., Ahmed, A., Gudi, A., Govind, A., Jauniaux, E.: Correlation of IVF outcomes and number of oocytes retrieved: a UK retrospective longitudinal observational study of 172 341 non-donor cycles. BMJ Open 13, e064711 (2023). https://doi.org/10.1136/bmjopen-2022-064711
Stehlik, E., Stehlik, J., Katayama, K.P., Kuwayama, M., Jambor, V., Brohammer, R., Kato, O.: Vitrification demonstrates significant improvement versus slow freezing of human blastocysts. Reprod. Biomed. Online 11, 53–57 (2005). https://doi.org/10.1016/s1472-6483(10)61298-9
Fishel, S., Campbell, A., Foad, F., Davies, L., Best, L., Davis, N., Smith, R., Duffy, S., Wheat, S., Montgomery, S., Wachter, A., Beccles, A.: Evolution of embryo selection for IVF from subjective morphology assessment to objective time-lapse algorithms improves chance of live birth. Reprod. Biomed. Online 40, 61–70 (2020). https://doi.org/10.1016/j.rbmo.2019.10.005
Cimadomo, D., Sosa Fernandez, L., Soscia, D., Fabozzi, G., Benini, F., Cesana, A., Dal Canto, M.B., Maggiulli, R., Muzzì, S., Scarica, C., Rienzi, L., De Santis, L.: Inter-centre reliability in embryo grading across several IVF clinics is limited: implications for embryo selection. Reprod. Biomed. Online 44, 39–48 (2022). https://doi.org/10.1016/j.rbmo.2021.09.022
Berntsen, J., Rimestad, J., Lassen, J.T., Tran, D., Kragh, M.F.: Robust and generalizable embryo selection based on artificial intelligence and time-lapse image sequences. PLoS ONE 17, e0262661 (2022). https://doi.org/10.1371/journal.pone.0262661
Paffoni, A., Reschini, M., Pisaturo, V., Guarneri, C., Palini, S., Viganò, P.: Should rescue ICSI be re-evaluated considering the deferred transfer of cryopreserved embryos in in-vitro fertilization cycles? A systematic review and meta-analysis. Reprod. Biol. Endocrinol. 19, 121 (2021). https://doi.org/10.1186/s12958-021-00784-3
Porgo, T.V., Moore, L., Assy, C., Neveu, X., Gonthier, C., Berthelot, S., Gabbe, B.J., Cameron, P.A., Bernard, F., Turgeon, A.F.: Development and validation of a hospital indicator of activity-based costs for injury admissions. Value Health. 24, 530–538 (2021). https://doi.org/10.1016/j.jval.2020.11.011
Busse, R., Schreyögg, J., Smith, P.C.: Variability in healthcare treatment costs amongst nine EU countries - results from the HealthBASKET project. Health Econ. 17, S1-8 (2008). https://doi.org/10.1002/hec.1330
Defourny, N., Hoozée, S., Daisne, J.-F., Lievens, Y.: Developing time-driven activity-based costing at the national level to support policy recommendations for radiation oncology in Belgium. J. Account. Public Policy 42, 107013 (2023). https://doi.org/10.1016/j.jaccpubpol.2022.107013
da Etges, A.P.B.S., Ruschel, K.B., Polanczyk, C.A., Urman, R.D.: Advances in value-based healthcare by the application of time-driven activity-based costing for inpatient management: a systematic review. Value Health. 23, 812–823 (2020). https://doi.org/10.1016/j.jval.2020.02.004
Copp, T., Kvesic, D., Lieberman, D., Bateson, D., McCaffery, K.J.: “Your hopes can run away with your realistic expectations”: a qualitative study of women and men’s decision-making when undergoing multiple cycles of IVF. Hum. Reprod. Open. 2020, hoaa059 (2020). https://doi.org/10.1093/hropen/hoaa059
ESHRE: Number of frozen treatment cycles continues to rise throughout the world, https://www.focusonreproduction.eu/article/ESHRE-News-22EIM, Accessed December 6, 2023
Dancet, E.A.F., Nelen, W.L.D.M., Sermeus, W., De Leeuw, L., Kremer, J.A.M., D’Hooghe, T.M.: The patients’ perspective on fertility care: a systematic review. Hum. Reprod. Update 16, 467–487 (2010). https://doi.org/10.1093/humupd/dmq004
Collins, J.: An international survey of the health economics of IVF and ICSI. Hum. Reprod. Update 8, 265–277 (2002). https://doi.org/10.1093/humupd/8.3.265
Connolly, M.P., Ledger, W., Postma, M.J.: Economics of assisted reproduction: access to fertility treatments and valuing live births in economic terms. Hum. Fertil. (Camb.) 13, 13–18 (2010). https://doi.org/10.3109/14647270903401747
Drummond, M., Sculpher, M.J., Claxton, K., Stoddart, G.L., Torrance, G.W.: Methods for the economic evaluation of health care programmes. Oxford University Press, London, England (2015)
Cassettari, L., Mosca, M., Mosca, R., Rolando, F., Costa, M., Pisaturo, V.: IVF cycle cost estimation using activity based costing and Monte Carlo simulation. Health Care Manag. Sci. 19, 20–30 (2016). https://doi.org/10.1007/s10729-014-9282-2
Eldenburg, L., Soderstrom, N., Willis, V., Wu, A.: Behavioral changes following the collaborative development of an accounting information system. Acc. Organ. Soc. 35, 222–237 (2010). https://doi.org/10.1016/j.aos.2009.07.005
Veiga, E., Olmedo, C., Sánchez, L., Fernández, M., Mauri, A., Ferrer, E., Ortiz, N.: Recalculating the staff required to run a modern assisted reproductive technology laboratory. Hum. Reprod. 37, 1774–1785 (2022). https://doi.org/10.1093/humrep/deac121
da Silva Etges, A.P.B., Cruz, L.N., Notti, R.K., Neyeloff, J.L., Schlatter, R.P., Astigarraga, C.C., Falavigna, M., Polanczyk, C.A.: An 8-step framework for implementing time-driven activity-based costing in healthcare studies. Eur. J. Health Econ. 20, 1133–1145 (2019). https://doi.org/10.1007/s10198-019-01085-8
Maussen, S., Cardinaels, E., Hoozée, S.: Costing system design and honesty in managerial reporting: an experimental examination of multi-agent budget and capacity reporting. Account. Organ. Soc. 112, 101541 (2024). https://doi.org/10.1016/j.aos.2024.101541
Maussen, S., Hoozée, S.: On the influence of task interruption and interactive time estimation on estimation error in time-based costing systems. Eur. Account. Rev. 31, 519–541 (2022). https://doi.org/10.1080/09638180.2020.1826339
Keel, G., Savage, C., Rafiq, M., Mazzocato, P.: Time-driven activity-based costing in health care: a systematic review of the literature. Health Policy 121, 755–763 (2017). https://doi.org/10.1016/j.healthpol.2017.04.013
Campanale, C., Cinquini, L., Tenucci, A.: Time-driven activity-based costing to improve transparency and decision making in healthcare: a case study. Qual. Res. Account. Manag. 11, 165–186 (2014). https://doi.org/10.1108/qram-04-2014-0036
Funding
This study was funded by DSW insurance company. Publication of study results was not contingent on sponsor’s approval.
Author information
Authors and Affiliations
Contributions
Conceptualization and supervision: ML, HJvE, KA, CGJMH, EJPvS. Material preparation and data collection: ML, EJPvS. Formal analysis; ML, HJvE, KA. First draft written by ML with input from HJvE, KA, CGJMH, EJPvS. Supplementary materials written and/or made by ML, EJPvS and CGJMH with input from HJvE and KA.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the ESHPM Research Ethics Review Committee (ETH122-0355) and the Reinier de Graaf Hospital (2022-032).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Leusder, M., van Elten, H.J., Ahaus, K. et al. Patient-level cost analysis of subfertility pathways in the Dutch healthcare system. Eur J Health Econ (2024). https://doi.org/10.1007/s10198-024-01744-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10198-024-01744-5