Abstract
Conventional Insemination (CI) and Intra-Cytoplasmic Sperm Injection (ICSI) are routinely used insemination methods in clinical Assisted Reproductive Technologies (ART) settings. However, the existing data on the developmental competence and implantation potential of CI and ICSI derived embryos are not unequivocal. This prospective study on 23 patients undergoing ART treatment explored whether the secretomes of CI- and ICSI-derived embryo differentially alter the expression of integrins (αv and β3 integrin) and MUCIN-1 (MUC-1) in a human endometrial epithelial cell line (Ishikawa). Immunocytochemical data demonstrated that the secretome of CI-derived top quality (GI) embryos induced higher (p < 0.05) expression of ɑv β3 compared to sibling ICSI derived G1 embryos in Ishikawa cells. Though, relative levels of the transcript for MUC-1, anti-adhesion molecule did not show a significant difference between the study groups, immunocytochemical analysis demonstrated significantly (p < 0.0001) higher expression of MUC-1 in cells treated with ICSI-derived embryo secretome, compared to that treated with CI -derived embryo secretome. These results suggest that secretomes from CI and ICSI embryos differentially modulate the endometrial cells in vitro. This hints at differences in the ability of CI- and ICSI- derived embryos to alter endometrial profile.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
Conventional Insemination (CI) and Intra-Cytoplasmic Sperm Injection (ICSI) are routinely used insemination methods in clinical Assisted Reproductive Technologies (ART) settings. Several reports recommend ICSI for attaining higher fertilization rate and better embryo yield to improve the cumulative pregnancy rate [1,2,3,4,5]. Nonetheless there exist sufficient data to suggest that ICSI is not helpful in achieving higher pregnancy or live birth rates, compared to CI [6,7,8,9,10]. Yet, ICSI is preferred insemination technique, in about 70% of fresh ART cycles, indicating the overuse of this method [8, 11,12,13].
Reports on the developmental competence and implantation potential of CI- and ICSI- derived embryos are contradictory [8, 14,15,16,17,18,19]. ICSI is reported to have a better clinical outcome than CI in couples with non-male factor infertility [20,21,22,23]. Several meta-analyses have inferred that implantation and live birth rates from CI-derived embryos are higher, compared to that resulting from ICSI [6, 17, 19], A recent study has also shown that compared to CI, ICSI results in a lower fertilization rate and lower rate of euploid embryos [24].
Bi-directional communication between blastocyst and endometrium is an important requisite for successful implantation and pregnancy. Studies using rodent [25,26,27] and primate models have demonstrated the ability of embryonic signals to modulate the endometrium [28,29,30]. The secretome of human embryos is also reported to modulate the endometrial cells at molecular level [31,32,33]. Further, human embryo secretome was found to promote proliferation of endometrial cells and modulate the expression of implantation- related genes [34]. However, these studies employed pooled spent culture media from embryos, irrespective of their quality. Hence it was not clear whether the alterations observed in the endometrial epithelial cells were induced by only good quality embryos or whether these changes were observed due to certain embryonic products, that are secreted independent of their quality.
A few strides have been made to analyse Spent Culture Medium (SCM) of CI- and ICSI- derived embryos to explore whether these embryos differ at molecular level. SCMs of CI- and ICSI- derived embryos from patients with moderate male factor infertility did not differ in terms of their metabolic profiles [35]. Our recent NMR-based study, also found metabolomic signatures of CI and ICSI derived embryos from non-male factor patients undistinguishable [36]. However, it is likely that NMR spectroscopy, probably failed to identify the low-abundant metabolites, differentially abundant in the secretome of CI- and ICSI- derived embryos [37, 38]. Though, developmentally and morphologically CI- and ICSI- derived embryos are comparable [39], differences have been reported in their transcriptomes, proteomes [24, 40], and epigenomes [41]. These alterations may have implications on the implantation potential of CI- and ICSI- derived embryos. It is likely that the secretomes from CI and ICSI derived embryos differentially trigger various signalling pathways and thereby differentially modulate the expression of implantation-related genes in endometrial cells.
To the best of our knowledge, there is no study that has employed a cell-based assay to compare the competency of CI- and ICSI- derived embryos to modulate endometrial epithelial cells. Hence we made an attempt to explore whether CI and ICSI- derived embryo secretomes differentially alter the expression of integrin ɑvβ3 and MUCIN-1 in human endometrial epithelial cell lines. Integrin ɑvβ3 is a receptivity marker that shows increased expression in the mid-secretory phase of menstrual cycle. Integrin is known to play a role if embryo attachment, angiogenesis as well as placental invasion into the maternal vasculature [42]. MUC-1, also receptivity marker, regulates implantation by inhibiting cell-to-cell adhesion. Local reduction of MUC-1 expression at attachment sites allows the blastocyst to implant and, MUC-1 expression is reported to be critical for the selection of high-quality embryos [43]. It was envisaged a comparison of the ability of secreted factors from CI- and ICSI- derived embryos to modify the endometrial epithelial cells will indirectly establish whether the molecular profiles of that CI- and ICSI- derived embryos are similar or dissimilar.
Methods
Study subjects
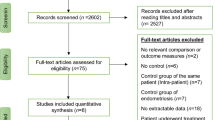
A total of 23 couples undergoing ART treatment at the University's infertility clinic were included in this prospective study. Approval from Institutional Ethics Committee (IEC1: 297/2022) was taken prior to the initiation of the study. Patients who signed the informed consent and qualified the following criteria were included in the study: i) women < 35 years of age ii) having no pelvic pathologies such as endometriosis or tubal abnormalities, as indicated by their medical history; ii) having regular menstrual cycles as disclosed in their medical history; iii) having no metabolic/endocrine system-related conditions, such as hyperprolactinemia or hypo/hyperthyroidism iv) partner’s semen characteristics classified as ‘normal’ as per the WHO 2010 reference range [44]. The demographic characteristics of the patients and clinical investigations details are summarized in Table 1.
Ovarian stimulation and oocyte retrieval
An antagonist protocol was performed during Controlled Ovarian Stimulation (COS). Recombinant FSH (rFSH, Gonal F®, Merck) was administered on day 2 of the cycle. Based on age, antral follicle count, and Anti-Mullerian Hormone level, initial dose of rFSH ranged from 225 to 450 IU/day. Thereafter, the rFSH dose was increased/decreased based on the ovarian response until the day prior to hCG administration. Pituitary down-regulation was accomplished by daily injection of the GnRH antagonist Citrotide ® 0.25 mg, (Merck), starting from Day 5 of the stimulation. Recombinant human chorionic gonadotropin (Ovitrelle® 250 mg, Merck Biopharma) was administered when at least four follicles had a mean diameter of 18 mm. Follicular aspiration was done under anesthesia using transvaginal ultrasonography. Aspirated oocyte cumulus complexes (OCC) were washed in Onestep medium (Vitromed GmbH, Germany; Cat No. V-OSM-20) and incubated at 37 °C under 6% CO2 for 2–3 h.
Fertilization and embryo assessment
Split insemination was performed using CI and ICSI techniques by randomly assigning the sibling Oocyte Cumulus Complexes (OCC). Insemination droplet (80 µL) having 15,000 to 20,000 spermatozoa from the processed fraction of the ejaculate was overlaid with oil (Vitromed GmbH, Germany; Cat No V-OIL-P100). Conventional Insemination (CI) was performed by transferring OCC to individual insemination droplet followed by co-incubation at 37 °C, 6% CO2, and 5% O2 in the MIRI® Multiroom incubator (ESCO Medical, Singapore). After 16–18 h, zona-bound spermatozoa and cumulus cells were completely removed by mechanical pipetting and multiple washing steps.
ICSI was performed by selecting single, motile, morphologically normal spermatozoon and injecting into a metaphase II oocyte using Olympus-Narishige workstation. Post ICSI, oocytes were washed and cultured individually in 30 µL Onestep medium droplet covered with oil. Fertilization evaluation was performed simultaneously 16–18 h after CI or ICSI and fertilized oocytes from each group were transferred to a freshly prepared 30 µL droplet of Onestep medium and incubated at 37 °C, 6% CO2, and 5% O2 in a MIRI® Multiroom incubator. On day 3, embryos were microscopically assessed from both the groups for cell number, blastomere regularity, and morphological defects as per the ESHRE consensus [45] and graded accordingly. Grade I embryos had stage-specific cell number and size, with < 10% fragmentation and had no multinucleation. Embryos were either selected for transfer or cryopreserved, based on the clinical indication.
Spent embryo culture medium (SCM) collection
SCMs of those that developed into optimal embryos were collected carefully by aspirating 30 µL from the droplet without oil contamination and placed individually into labelled sterile cryovials, snap frozen in liquid nitrogen, and then stored at -80 °C [36]. One medium droplet without the embryo, maintained under identical conditions, was used as the medium control (MC) for every experimental group (CI or ICSI) from every patient.
Maintenance of cell lines
Ishikawa endometrial epithelial cell line (Sigma-Aldrich) derived from human endometrial adenocarcinoma was used. Ishikawa cell line was propagated in complete Dulbecco’s Minimal Essential Medium (DMEM)/F-12 medium supplemented with 10% fetal bovine serum (FBS) (Thermo Fisher Scientific, USA; Cat No. 10082147), 100 units/mL penicillin and 100 µg/mL streptomycin (Gibco™, Grand Island, USA; Cat No. 15140122).
Cell culture
Experiments related to cell culture, SCM treatment and subsequent analysis were performed at Indian Council of Medical Research (ICMR)-National Institute for Research in Reproductive and Child Health (NIRRCH), Mumbai. Ishikawa cells were seeded at a density of 1 × 104 per well, in a 48- well culture plate (Cat No.150687) over a coverslip [46]. The cell density was kept uniform for all the experiments. Post 16 h, culture media was replaced with 240 µl of medium supplemented with 10 μl of SCM or MC. Cells were grown for 72 h and monitored regularly using an inverted phase-contrast microscope (Nikon eclipse Ti-S).
Immunocytochemistry
Expression levels of a heterodimer of two integrins (ɑv and β3) and anti-adhesion protein, Mucin-1 (MUCIN-1) were assessed in Ishikawa cells treated with CI- or ICSI- derived SCMs. Cells grown on coverslips after 72 h treatment were fixed in 2% Paraformaldehyde (PFA), 0.05% glutaraldehyde and 120 mM sucrose for 30 min at room temperature and washed with 1 × PBS followed by blocking with 1% BSA for 30 min [34]. Cells were incubated with mouse antibodies against ɑv β3 integrin heterodimer (1:25), conjugated to Alexa Fluor® 488 (Santa Cruz Biotechnology Inc, USA; Cat No. SC-7312). In another set of experiments, cells were stained with mouse antibodies against human Mucin-1 (1:75) (Santa Cruz Biotechnology Inc, USA; Cat No. SC- 6827) for 16 h at 4 °C. After three 1 × PBS washes, cells stained with antibodies against MUC-1 were incubated with goat anti-mouse IgG conjugated to Alexa Fluor 488 (1:100) (Thermo Fisher Scientific, USA; Cat. No. A11001) for 1 h at 37° C. Finally, cells were stained with DAPI (4’, 6-Diamidino-2-phenylindole) (Roche, Basel, Switzerland; Cat No. 10236276001) and mounted with Vectashield antifade mounting medium (VECTASHIELD® Antifade Mounting Medium, USA; Cat. No. H-1000–10).
Images of immunostained cells were captured using confocal laser scanning microscope (Olympus, Germany) in XY plane using 60 × objective. Five fields for each sample were selected. Image analysis was performed by determining the intensities for immunoreactive antigens in Ishikawa cells using the image analysis software Image J. The raw integrated density (RawIntDen) per field was determined by calculating the average of the staining intensities of each cell in that particular field. Integrated optical density (IOD) for each sample was calculated as the mean of the RawIntDen of all the fields. Background settings were adjusted by observing the negative control wherein cells were incubated with 1 × PBS, instead primary antibody.
Total RNA isolation, cDNA synthesis, and gene expression analysis
Total RNA was extracted from cells treated with SCMs from CI, ICSI or MC group using RNAqueous micro kit (Ambion, Life Technologies, USA; Cat No. AM1931) according to the manufacturer’s instructions. 1 µg of total RNA was reverse transcribed using random hexamers by high-capacity cDNA RT kit (Applied biosystems, USA; Cat No. 4368814) according to the manufacturer`s protocol. Quantitative real-time polymerase chain reaction (RT qPCR) was carried out using Premix Ex Taq kit (TaKaRa Bio, Japan; Cat No. RR390A), in StepOne™ Real-Time PCR System (Thermo Fisher Scientific, USA). 1 µL cDNA was used to determine the relative levels of Integrin ɑv, Integrin β3 and MUCIN-1 transcripts in cells treated with the SCMs from embryos, compared to MC treated embryos using Premix Ex Taq kit (TaKaRa Bio, Japan; Cat No. RR390A) QuantStudio™ 5 Real-Time PCR System (Thermo Fisher Scientific, USA). TaqMan assays (Thermo Fisher Scientific, USA) ITGB3 (Hd01001469_m1), ITGAV (Hs00233808_m1) and MUC1 (Hs0059357_m1) taqman assays were used. Transcript levels of integrin ɑv, integrin β3 and MUC-1 gene were normalized against the endogenous housekeeping gene 18S rRNA [47]. ΔCt values were calculated as the difference in the threshold cycles between the target genes and reference genes ΔCt = Ct (target gene) – Ct (reference gene) for each sample.
Statistical analysis
The demographic and clinical characteristics of the patients enrolled are represented as mean ± standard deviation of the mean (mean ± SD) or median (IQR) after verification of the normality assumption (using the Shapiro–Wilk test). Univariate analysis of the embryological characteristics was implemented using GraphPad Prism 8 (GraphPad Prism software, CA, USA). Based on assessment of the normality assumption and the homogeneity of variance assumption (using the Levene's test) for the parameters across the groups, appropriate statistical inference methods were implemented using Jamovi 2.3.24 (graphical user interface for R programming). When both the assumptions are satisfied, Fisher's ANOVA with Tukey's post-hoc comparison was utilized to facilitate comparisons of parameters across multiple groups. Kruskal Wallis ANOVA with Dwass-Steel-Critchlow-Fligner post-hoc comparison was used in scenarios wherein a violation of normality and homogeneity of variance assumption was observed. The level of significance was set at 5% throughout the study. Furthermore, histograms were plotted using GraphPad Prism 8 (GraphPad Prism software, CA, USA). The assumption of data normality for correlation analysis was tested using Shapiro–Wilk test. Correlation analysis was performed using the spearman rank correlation coefficient since data was not distributed normally. The results were considered as statistically significant at p < 0.05. In the present study Fisher's ANOVA with Tukey's post-hoc comparison was used in the present study for the following parameters: for comparing transcript levels of integrin ɑv, integrin β3 and MUC-1 between two groups. For Immunocytochemistry results, Kruskal Wallis ANOVA with Dwass-Steel-Critchlow-Fligner post-hoc comparison was used.
Results
Patient characteristics, fertilization outcome and embryo quality
Demographics and clinical characteristics of patients (n = 23) included in this study are shown in Table 1. Embryological data are presented in Table 2. Though the average number of oocytes used for insemination in the two groups was comparable, the fertilization rate was significantly higher in ICSI group (p < 0.05). The cleavage rate and embryo quality on day 3 were comparable between the two groups.
SCM of human embryos upregulated the expression of integrin (ɑv β3) in Ishikawa cells
Relative levels of Integrin ɑv and β3 transcripts were assessed using Real-time qRT PCR of RNA extracted from Ishikawa cells treated with SCMs derived from CI or ICSI derived embryos of grade I or grade II (n = 5 each). Cells treated with embryo SCMs had significantly lower ΔCt value for integrin ɑv compared to cells treated with media alone, indicating that the embryo secretome from both groups (ICSI- or CI- derived embryo) led to a significant by (p < 0.0001) higher expression of αv transcript compared to the cells treated with media alone (MC). Further, this effect was observed irrespective of the type (CI/ICSI) or grade of embryo (Fig. 1A). Thus, a significant modulation in the levels of integrin ɑv transcript by embryo SCMs occurred irrespective of the embryo quality and insemination techniques. On the other hand, integrin β3 transcript levels did not differ significantly between MC and CI groups. Interestingly ICSI group showed significantly (p < 0.05) higher level of β3 transcripts compared to MC group.
Relative levels of ɑv (A) and β3 (B) trancripts in Ishikawa cells treated with the secretomes (SCM) of human embryos derived (by CI and ICSI) of grade I and grade II (n = 5 each). Total RNA extracted from Ishikawa cells treated with media alone (MC) or SCM of CI/ICSI sibling embryos was converted to cDNA and amplified for assessing the levels of ɑv and β3 transcripts. 18S rRNA was used as a housekeeping gene. Taqman primer probes for the gene of interest (ɑv and β3) and housekeeping gene 18S rRNA were used in real time RT-PCR assays. ΔCt (threshold cycle) were determined. ΔCt was calculated as Ct (gene of interest)- Ct (housekeeping gene). *p < 0.05; ***p < 0.0001
To validate these observations, immunolocalization of integrin (ɑvβ3) protein was carried out (Fig. 2). The cytoplasmic expression of integrin (ɑvβ3) in epithelial cells treated with the SCM from CI derived embryos (G1) was significantly (p < 0.05) higher than that detected in the MC treated cells (n = 11) (p < 0.05) (Fig. 2A). In contrast, integrin (ɑvβ3) expression was significantly (p < 0.05) lower in the ICSI group (II) as compared to MC group.
Immunolocalization of integrin (ɑvβ3) heterodimer in Ishikawa cells treated with SCM. A Relative cytoplasmic expression of integrin (ɑvβ3) in Ishikawa cells treated with SCM from grade I (21 GI-CI & 24 GI-ICSI) and II (16 GII-CI & 16 GII-ICSI) embryos derived from CI or ICSI techniques along with MC (n = 11). *p < 0.05; ***p < 0.0001. B Immunocytochemical localization to depict the localization of integrin (ɑv β3) heterodimer in Ishikawa cells treated with SCM of MC or GI and GII embryos derived from CI and ICSI
Further, when compared between the cultures stimulated with SCM from GI (21 GI-CI & 24 GI-ICSI) and GII (16 GII-CI & 16 GII-ICSI) embryos, GI embryo secretome group showed significantly (p < 0.0001) higher expression than that observed in GII group. Importantly, ICSI-derived GI embryo secretome resulted in a significantly (p < 0.05) lower expression of αvβ3 heterodimer in Ishikawa cells compared to CI-derived GI embryos. Representative images of Ishikawa cells demonstrating expression of heterodimer integrin (ɑvβ3) are presented in Fig. 2B. Overall, the secretome of CI-derived embryo was found to induce higher expression of ɑvβ3 heterodimer compared to secretome of sibling ICSI-derived embryo.
Further, a significant (p < 0.001) positive correlation (Spearman correlation coefficient, r = 0.7328) was found for integrated optical density units for immunoreactive ɑvβ3 localization in Ishikawa cells between the SCMs from CI- and ICSI-derived sibling embryos (Fig. 3). Thus, treatment with the secretomes of CI- and ICSI-derived embryos from sibling oocytes led to higher expression of ɑvβ3 in Ishikawa cells. However, intensity of immunolocalized integrin (ɑvβ3) in endometrial cells treated with the SCM from CI-derived embryo was higher than that induced by the respective sibling ICSI-derived embryo.
Correlation of Integrin (ɑvβ3) heterodimer expression observed in Ishikawa cells treated with the SCM of grade I sibling human embryos derived by CI and ICSI (n = 17 sibling embryo pairs). Integrated optical density of immunoreactive integrin (ɑvβ3) as indicator of relative cytoplasmic expression of ɑvβ3 in Ishikawa cell treated with SCM of grade I sibling human embryos derived by CI and ICSI technique. T Spearman Correlation Coefficient, r between the two groups was 0.7328. p < 0.001
Human SCM induced expression of MUC-1 in Ishikawa cells
Relative expression of MUC-1 transcripts did not differ significantly between the study groups of grade I and grade II embryos secretome treated cells (n = 5 each)(Fig. 4). However, immunocytochemistry data showed four-fold higher expression of MUC-1 in Ishikawa cells treated with SCM from GII-ICSI group compared to corresponding MC, GI-ICSI(21 GI-CI & 24 GI-ICSI) and GII-CI (16 GII-CI & 16 GII-ICSI) groups (p < 0.0001; Fig. 5A). Representative images of cells immunostained for MUC-1 are shown in Fig. 5B.
Relative levels of Mucin-1 (MUC-1) transcripts in Ishikawa cells treated with the SCMs of human embryos derived (by CI and ICSI) of grade I and grade II (n = 5 each). Total RNA extracted from Ishikawa cells treated with media alone (MC) or SCM of CI/ICSI sibling embryos was converted to cDNA and amplified for assessing the level MUC-1 transcript. 18S rRNA was used as a housekeeping gene. Taqman primer probes for MUC-1 gene and housekeeping gene 18S rRNA were used in real time RT-PCR assays. Δ Ct (threshold cycle) were determined. Δ Ct was calculated as Ct (gene of interest)- Ct (housekeeping gene)
Immunolocalization of Mucin-1 (MUC-1) in Ishikawa cells treated with SCM. A Relative cytoplasmic expression of MUCIN-1 (MUC-1) in Ishikawa cells treated with SCM from grade I (21 GI-CI & 24 GI-ICSI) and II (16 GII-CI & 16 GII-ICSI) embryos derived from CI or ICSI techniques along with MC (n = 11), ***p < 0.0001. B Immunocytochemical localization to depict the localization of Mucin-1 (MUC-1) in Ishikawa cells treated with SCM of MC or GI and GII embryos derived from CI and ICSI
Discussion
Currently there is no consensus on the quality, implantation rates and pregnancy outcome of cycles wherein embryos derived by different insemination techniques (CI and ICSI) are transferred [20,21,22,23, 48]. Nonetheless, it is well established that autocrine and/or paracrine factors released by an embryo influence the surrounding microenvironment [49, 50] and also endometrial profile. We hypothesise that the secretomes of CI and ICSI derived embryos may have differential ability to modulate endometrial epithelial cells. Towards this sibling embryo secretomes were used to minimize confounding factors. Our data suggested differential response of endometrial epithelial cells to the secretomes of CI- and ICSI- derived embryos.
Results from the present study demonstrated that fertilization rate was higher in the ICSI group. This is in contrast to the other reports where in higher fertilization rates were observed when CI was used in non-male factor infertility patients [2, 51, 52]. It is important to note that sibling oocytes were used to ensure that all in-vitro conditions except insemination techniques were kept identical between the two groups in this study.
In vitro studies have shown that human SCM secretome influences the endometrial cells [31,32,33] either by increasing the cell proliferation or by modulating the expression of implantation-related genes [34, 53]. Clinically, embryo transfer along with its SCM has been shown to significantly improved the pregnancy outcome [53]. Hence, it is possible that the embryo secreted factors may favour embryo-endometrial interactions and improve implantation. Though the exact mechanism is not completely elucidated, Giacomini et al., (2017) demonstrated human embryos secrete extracellular vesicles that can be taken-up easily by the endometrial cells.
Integrins cell adhesion molecules, are known to have well-established role in cell invasion, migration, and embryo- endometrial interactions [54,55,56]. Integrins play a key role in mammalian implantation [57,58,59,60,61]. Therefore, we opted to investigate whether endometrial integrin expression is differentially altered in response to the secretomes of CI and ICSI derived embryos. Ishikawa cell line was selected as it has characteristics of both glandular and luminal epithelium [62] and is widely considered a good model for studying normal endometrial function. Importantly, Ishikawa cells express many enzymes and structural proteins found in normal endometrium [63], along with functional steroid receptors.
Ishikawa cells treated with the SCMs of CI- and ICSI- derived embryos showed higher levels of ɑv transcript, compared to the cells treated with media alone. This suggests that human embryo secretome has factors that are capable of upregulating the expression of integrin ɑv transcript in endometrial epithelial cells. These results are in contrast to the previous observations. Our previous in-vitro studies [34] demonstrated comparable expression of ɑv integrin protein in Ishikawa cells treated with the SCM of human IVF embryos and cells treated with media alone. β3 protein expression, on the other hand, was found significantly higher in the cells treated with the SCM of IVF embryos, compared to these treated with media alone. The present study however, demonstrated significantly higher expression of ɑv transcript in all study groups, as compared to control group and higher β3 transcript levels only in ICSI group, compared to the control group. This discordance can be attributed to a different study design adopted in the present study. Firstly, in contrast to our previous study, expression of ɑvβ3 protein (a functional heterodimer) was investigated in cells treated with the secretome of single embryos, rather than a pooled secretome of different embryos of unknown quality. It is likely that the pooled conditional media of human embryos failed to cause a significant increase in the expression of ɑv protein because of potential dilution of factors causing ɑv integrin expression. Further β3 transcript levels were significantly increased in response to the secretome of ICSI embryos. No significant change observed in the levels of β3 transcript in response to the secretome of CI embryos in the present study may be attributed to discordance between RNA and protein expression for β3 integrin in cells treated with CI embryo secretomes. Further, it is likely that significantly higher localization of ɑvβ3 heterodimer protein observed in Ishikawa cells, treated with the secretomes of CI and ICSI derived embryos resulted from either higher expression of ɑv protein or due to preferential dimerization of ɑv and β3 proteins.
Interestingly, when compared within CI or ICSI groups, ɑvβ3 heterodimer localization was always higher (p < 0.05) in grade I embryo secretome treated cells than in grade II secretome treated cells. Further, a significant positive correlation between ɑvβ3 expression induced by grade I CI- and ICSI-derived embryos from sibling oocytes revealed that both, CI- and ICSI-derived embryos from sibling oocytes have the potential to induce Integrin ɑvβ3 expression. However, integrated optical density values of immunoreactive Integrin ɑvβ3 was higher in Ishikawa cells treated with the SCM from GI-CI than in cells treated with the SCM from GI-ICSI.
Mucin 1 (MUC1) is a membrane-associated protein, highly expressed in luminal and glandular epithelium on LH + 7 day [64, 65] and disappears at the site of embryo attachment in response to blastocyst-derived factors [66, 67]. Patients with the history of recurrent implantation failure are reported to have higher endometrial MUC-1 expression [68, 69]. In this study, GII-ICSI embryo group demonstrated significantly higher expression of MUC-1, compared to the control group. This increase in MUC-1 protein was paralleled by a similar increase at the transcript level. These observations hint at differential ability of CI and ICSI embryos to modulate endometrial epithelium. It has been shown that CI and ICSI can differentially influence embryonic gene expression [40, 70] More studies are warranted to elucidate the mechanism by which embryo secreted factors modify the endometrial expression of ɑvβ3 and MUC-1. Certain cytokines such as interferon gamma (IFNγ) and tumor necrosis factor alpha (TNF-α) have been shown to stimulate the expression of MUC-1 in breast epithelial cells [71], whereas transforming growth factor beta-1 (TGF-β1)-mediated upregulation of ɑvβ3 was reported in peritoneal fibroblasts [72]. The presence of these cytokines has been reported in embryo conditioned medium [73] and are known to play critical role in embryo implantation and pregnancy. Further studies are warranted to decipher whether the embryo-derived IFNγ, TNF-α and TGF-β1 modulate the expression of uterine ɑvβ3 and MUC1.
A successful implantation needs a competent embryo, a receptive endometrium and an effective cross-talk between them. It is well established that endocrine factors, endometrial pathology [74], and immunological factors [75], influence the endometrial receptivity and affect the implantation potential. However the effects of fertilization mechanisms on the implantation remain poorly understood. From the clinical ART perspectives, the observations made in this study provide new insights into possible influence of laboratory manipulation of gametes on embryo-endometrial interaction. Observations from the present study also hint at clinical opportunities to assess the embryo competence for implantation.
The strengths of this study are the use of secretomes of CI and ICSI derived embryos from sibling oocytes. To our knowledge, this approach has not been adopted to elucidate the effect of CI and ICSI on embryo quality. Since the secretomes from day 3 embryos were utilized, there is a scope to develop non-invasive biomarker to predict the embryo implantation potential. The limitations of our study are i) lack of data on the pregnancy outcome due to transfer of more than one embryo to patients either from CI or ICSI cohort ii) lack of data on embryonic gene expression due to ethical restrictions. Genetic testing of the embryos would have provided evidence on the association between the secretome and ploidy status of the embryos which was not done in our study.
Conclusion
A cell-based in vitro approach, revealed that CI- and ICSI- derived embryo secretomes modulate the expression of endometrial cells in vitro. Therefore, it is possible that embryo-endometrial interaction and implantation post-embryo transfer are also different for CI- and ICSI- derived embryos. Since the existing data on the clinical outcome between the two insemination techniques in non-male factor infertility are contradictory, the observation made, especially in the context of ɑvβ3 protein localization, favours CI. Hence, ICSI technique should be utilized for the indication it was developed for, and not as a first-line insemination method for patients with non-male factor infertility.
Data availability
The data and material that support the findings of this study are available from the corresponding author upon request.
References
Staessen C, Camus M, Clasen K, De Vos A, Van Steirteghem A. Conventional in-vitro fertilization versus intracytoplasmic sperm injection in sibling oocytes from couples with tubal infertility and normozoospermic semen. Hum Reprod. 1999;14:2474–9.
Tannus S, Son WY, Gilman A, Younes G, Shavit T, Dahan MH. The role of intracytoplasmic sperm injection in non-male factor infertility in advanced maternal age. Hum Reprod. 2017;32:119–24.
Sustar K, Rozen G, Agresta F, Polyakov A. Use of intracytoplasmic sperm injection (ICSI) in normospermic men may result in lower clinical pregnancy and live birth rates. Aust N Z J Obstet Gynaecol. 2019;59:706–11.
Abbas AM, Hussein RS, Elsenity MA, Samaha II, El Etriby KA, Abd El-Ghany MF, Khalifa MA, Abdelrheem SS, Ahmed AA, Khodry MM. Higher clinical pregnancy rate with in-vitro fertilization versus intracytoplasmic sperm injection in treatment of non-male factor infertility: Systematic review and meta-analysis. J Gynecol Obstet Hum Reprod. 2020;49: 101706.
Sunderam S, Boulet SL, Kawwass JF, Kissin DM. Comparing fertilization rates from intracytoplasmic sperm injection to conventional in vitro fertilization among women of advanced age with non-male factor infertility: a meta-analysis. Fertil Steril. 2020;113:354-363.e1.
Bhattacharya S, Hamilton MP, Shaaban M, Khalaf Y, Seddler M, Ghobara T, Braude P, Kennedy R, Rutherford A, Hartshorne G, Templeton A. Conventional in-vitro fertilisation versus intracytoplasmic sperm injection for the treatment of non-male-factor infertility: a randomised controlled trial. Lancet. 2001;357:2075–9.
van Rumste MM, Evers JL, Farquhar CM. ICSI versus conventional techniques for oocyte insemination during IVF in patients with non-male factor subfertility: a Cochrane review. Hum Reprod. 2004;19:223–7.
Boulet SL, Mehta A, Kissin DM, Warner L, Kawwass JF, Jamieson DJ. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA. 2015;313:255–63.
Grimstad FW, Nangia AK, Luke B, Stern JE, Mak W. Use of ICSI in IVF cycles in women with tubal ligation does not improve pregnancy or live birth rates. Hum Reprod. 2016;31:2750–5.
Iwamoto A, Van Voorhis BJ, Summers KM, Sparks A, Mancuso AC. Intracytoplasmic sperm injection vs. conventional in vitro fertilization in patients with non-male factor infertility. Fertil Steril. 2022;118:465–72.
Dyer S, Chambers GM, de Mouzon J, Nygren KG, Zegers-Hochschild F, Mansour R, Ishihara O, Banker M, Adamson GD. International Committee for Monitoring Assisted Reproductive Technologies world report: Assisted Reproductive Technology. 2009 and 2010. Hum Reprod. 2008;31:1588–609.
De Geyter C, Calhaz-Jorge C, Kupka MS, Wyns C, Mocanu E, Motrenko T, Scaravelli G, Smeenk J, Vidakovic S, Goossens V; European IVF-monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). ART in Europe. results generated from European registries by ESHRE: The European IVF-monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod. 2014;2018(33):1586–601.
Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. Intracytoplasmic sperm injection (ICSI) for non-male factor indications: a committee opinion. Fertil Steril. 2020;114:239–245. https://doi.org/10.1016/j.fertnstert.2020.05.032.
Aboulghar MA, Mansour RT, Serour GI, Sattar MA, Amin YM. Intracytoplasmic sperm injection and conventional in vitro fertilization for sibling oocytes in cases of unexplained infertility and borderline semen. J Assist Reprod Genet. 1996;13:38–42.
Maman E, Geva LL, Yerushalmi G, Baum M, Dor J, Hourvitz A. ICSI increases ongoing pregnancy rates in patients with poor response cycle: multivariate analysis of 2819 cycles. Reprod Biomed Online. 2012;25:635–41.
Farhi J, Cohen K, Mizrachi Y, Weissman A, Raziel A, Orvieto R. Should ICSI be implemented during IVF to all advanced-age patients with non-male factor subfertility? Reprod Biol Endocrinol. 2019;17:30.
Geng T, Cheng L, Ge C, Zhang Y. The effect of ICSI in infertility couples with non-male factor: a systematic review and meta-analysis. J Assist Reprod Genet. 2020;37:2929–45.
Chamayou S, Ragolia C, Alecci C, Storaci G, Romano S, Sapienza R, Maglia E, Liprino A, Cardea C, Fichera M, Guglielmino A. More blastocysts are produced from fewer oocytes in ICSI compared to IVF - results from a sibling oocytes study and definition of a new key performance indicator. Reprod Biol Endocrinol. 2021;19:116.
Huang JX, Gao YQ, Chen XT, Han YQ, Song JY, Sun ZG. Impact of intracytoplasmic sperm injection in women with non-male factor infertility: A systematic review and meta-analysis. Front Reprod Health. 2022;4:1029381.
Komsky-Elbaz A, Raziel A, Friedler S, Strassburger D, Kasterstein E, Komarovsky D, Ron-El R, Ben-Ami I. Conventional IVF versus ICSI in sibling oocytes from couples with endometriosis and normozoospermic semen. J Assist Reprod Genet. 2013;30:251–7.
Li Z, Wang AY, Bowman M, Hammarberg K, Farquhar C, Johnson L, Safi N, Sullivan EA. ICSI does not increase the cumulative live birth rate in non-male factor infertility. Hum Reprod. 2018;33:1322–30.
Drakopoulos P, Garcia-Velasco J, Bosch E, Blockeel C, de Vos M, Santos-Ribeiro S, Makrigiannakis A, Tournaye H, Polyzos NP. ICSI does not offer any benefit over conventional IVF across different ovarian response categories in non-male factor infertility: a European multicenter analysis. J Assist Reprod Genet. 2019;36:2067–76.
Supramaniam PR, Granne I, Ohuma EO, Lim LN, McVeigh E, Venkatakrishnan R, Becker CM, Mittal M. ICSI does not improve reproductive outcomes in autologous ovarian response cycles with non-male factor subfertility. Hum Reprod. 2020;35:583–94.
Patel K, Vaughan DA, Rodday AM, Penzias A, Sakkas D. Compared with conventional insemination, intracytoplasmic sperm injection provides no benefit in cases of nonmale factor infertility as evidenced by comparable euploidy rate. Fertil Steril. 2023;120:277–86.
Lefèvre P, Campos DB, Murphy BD. Talk to me: the embryo dictates gene expression by the endometrium. Endocrinology. 2007;148:4170–2.
Spencer TE, Sandra O, Wolf E. Genes involved in conceptus-endometrial interactions in ruminants: insights from reductionism and thoughts on holistic approaches. Reproduction. 2008;135:165–79.
Koo HS, Yoon MJ, Hong SH, Ahn J, Cha H, Lee D, Ko JE, Kwon H, Choi DH, Lee KA, Ko JJ, Kang YJ. CXCL12 enhances pregnancy outcome via improvement of endometrial receptivity in mice. Sci Rep. 2021;11:7397.
Cameo P, Srisuparp S, Strakova Z, Fazleabas AT. Chorionic gonadotropin and uterine dialogue in the primate. Reprod Biol Endocrinol. 2004;2:50.
Fazleabas AT, Kim JJ, Strakova Z. Implantation: embryonic signals and the modulation of the uterine environment–a review. Placenta. 2004;25 Suppl A:S26-31.
Strakova Z, Mavrogianis P, Meng X, Hastings JM, Jackson KS, Cameo P, Brudney A, Knight O, Fazleabas AT. In vivo infusion of interleukin-1beta and chorionic gonadotropin induces endometrial changes that mimic early pregnancy events in the baboon. Endocrinology. 2005;146:4097–104.
Dominguez F, Gadea B, Mercader A, Esteban FJ, Pellicer A, Simón C. Embryologic outcome and secretome profile of implanted blastocysts obtained after coculture in human endometrial epithelial cells versus the sequential system. Fertil Steril. 2010;93:774-782.e1.
Capalbo A, Ubaldi FM, Cimadomo D, Noli L, Khalaf Y, Farcomeni A, Ilic D, Rienzi L. MicroRNAs in spent blastocyst culture medium are derived from trophectoderm cells and can be explored for human embryo reproductive competence assessment. Fertil Steril. 2016;105:225-235.e3.
Giacomini E, Vago R, Sanchez AM, Podini P, Zarovni N, Murdica V, Rizzo R, Bortolotti D, Candiani M, Viganò P. Secretome of in vitro cultured human embryos contains extracellular vesicles that are uptaken by the maternal side. Sci Rep. 2017;7:5210.
Nimbkar-Joshi S, Katkam RR, Chaudhari UK, Jacob S, Manjramkar DD, Metkari SM, Hinduja I, Mangoli V, Desai S, Kholkute SD, Puri CP, Sachdeva G. Endometrial epithelial cell modifications in response to embryonic signals in bonnet monkeys (Macaca radiata). Histochem Cell Biol. 2012;138:289–304.
Leary C, Sturmey RG. Metabolic profile of in vitro derived human embryos is not affected by the mode of fertilization. Mol Hum Reprod. 2020;26:277–87.
Jijo A, Cheredath A, Uppangala S, Lakshmi RV, Joseph D, Meitei HY, Asampille G, Kumar P, Gowda GAN, Kalthur G, Kovacic B, Adiga SK. ICSI in non-male factor infertility patients does not alter metabolomic signature in sibling embryos as evidenced by sensitivity enhanced nuclear magnetic resonance (NMR) spectroscopy. PLoS ONE. 2022;17: e0273321.
Burz DS, Breindel L, Shekhtman A. Improved sensitivity and resolution of in-cell NMR spectra. Methods Enzymol. 2019;621:305–28.
Kang C. Applications of In-Cell NMR in Structural Biology and Drug Discovery. Int J Mol Sci. 2019;20:139.
Fan W, Li SW, Li L, Huang Z, Ma Q, Wang Y, Xiao Z. Outcome of conventional IVF and ICSI on sibling oocytes in the case of isolated teratozoospermia. J Assist Reprod Genet. 2012;29:905–10.
Bridges PJ, Jeoung M, Kim H, Kim JH, Lee DR, Ko C, Baker DJ. Methodology matters: IVF versus ICSI and embryonic gene expression. Reprod Biomed Online. 2011;23:234–44.
Qiao J, Chen Y, Yan LY, Yan J, Liu P, Sun QY. Changes in histone methylation during human oocyte maturation and IVF- or ICSI-derived embryo development. Fertil Steril. 2010;93:1628–36.
Illera MJ, Lorenzo PL, Gui YT, Beyler SA, Apparao KB, Lessey BA. A role for alphavbeta3 integrin during implantation in the rabbit model. Biol Reprod. 2003;68:766–71.
Zarei R, Aboutorabi R, Rashidi B, Eskandari N, Nikpour P. Evaluation of vascular endothelial growth factor A and leukemia inhibitory factor expressions at the time of implantation in diabetic rats following treatment with Metformin and Pioglitazone. Int J Reprod Biomed. 2020;18:713–22.
World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 5th ed. Cambridge: Cambridge University Press; 2010.
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26:1270–83. https://doi.org/10.1093/humrep/der037.
Bane K, Desouza J, Rojewale A, Katkam RR, Fernandes G, Sawant R, Dudhedia U, Warty N, Chauhan A, Chaudhari U, Gajbhiye R, Sachdeva G. Dysregulation of X-ray repair cross-complementing 4 expression in the eutopic endometrium of women with endometriosis. Reproduction. 2022;163:95–105.
Bane K, Desouza J, Shetty D, Choudhary P, Kadam S, Katkam RR, Fernandes G, Sawant R, Dudhedia U, Warty N, Chauhan A, Chaudhari U, Gajbhiye R, Sachdeva G. Endometrial DNA damage response is modulated in endometriosis. Hum Reprod. 2021;36:160–74.
De Bantel-Finet A, Arbo E, Colombani M, Darné B, Gallot V, Grzegorczyk-Martin V, Languille S, Fréour T. Does intracytoplasmic sperm injection improve live birth rate when compared with conventional in vitro fertilization in non-male factor infertility? A systematic review and meta-analysis. F&S Reviews. 2021;3:57–68.
Ebner T, Shebl O, Moser M, Mayer RB, Arzt W, Tews G. Group culture of human zygotes is superior to individual culture in terms of blastulation, implantation and life birth. Reprod Biomed Online. 2010;21:762–8.
Restelli L, Paffoni A, Corti L, Rabellotti E, Mangiarini A, Viganò P, Somigliana E, Papaleo E. The strategy of group embryo culture based on pronuclear pattern on blastocyst development: a two center analysis. J Assist Reprod Genet. 2014;31:1629–34.
Luna M, Bigelow C, Duke M, Ruman J, Sandler B, Grunfeld L, Copperman AB. Should ICSI be recommended routinely in patients with four or fewer oocytes retrieved? J Assist Reprod Genet. 2011;28:911–5.
Shuai HL, Ye Q, Huang YH, Xie BG. Comparison of conventional in vitro fertilisation and intracytoplasmic sperm injection outcomes in patients with moderate oligoasthenozoospermia. Andrologia. 2015;47:499–504.
Luddi A, Pavone V, Governini L, Capaldo A, Landi C, Ietta F, Paccagnini E, Morgante G, De Leo V, Piomboni P. Emerging role of embryo secretome in the paracrine communication at the implantation site: a proof of concept. Fertil Steril. 2021;115:1054–62.
Aplin JD, Jones CJ, McGinlay PB, Croxatto HB, Fazleabas AT. Progesterone regulates glycosylation in endometrium. Biochem Soc Trans. 1997;25:1184–7.
Kimber SJ, Spanswick C. Blastocyst implantation: the adhesion cascade. Semin Cell Dev Biol. 2000;11:77–92.
Hood JD, Cheresh DA. Role of integrins in cell invasion and migration. Nat Rev Cancer. 2002;2:91–100.
Sutherland AE, Calarco PG, Damsky CH. Developmental regulation of integrin expression at the time of implantation in the mouse embryo. Development. 1993;119:1175–86.
Bowen JA, Bazer FW, Burghardt RC. Spatial and temporal analyses of integrin and Muc-1 expression in porcine uterine epithelium and trophectoderm in vivo. Biol Reprod. 1996;55:1098–106.
Lessey BA, Ilesanmi AO, Lessey MA, Riben M, Harris JE, Chwalisz K. Luminal and glandular endometrial epithelium express integrins differentially throughout the menstrual cycle: implications for implantation, contraception, and infertility. Am J Reprod Immunol. 1996;35:195–204.
Kimmins S, MacLaren LA. Cyclic modulation of integrin expression in bovine endometrium. Biol Reprod. 1999;61:1267–74.
Johnson GA, Bazer FW, Jaeger LA, Ka H, Garlow JE, Pfarrer C, Spencer TE, Burghardt RC. Muc-1, integrin, and osteopontin expression during the implantation cascade in sheep. Biol Reprod. 2001;65:820–8.
Mo B, Vendrov AE, Palomino WA, DuPont BR, Apparao KB, Lessey BA. ECC-1 cells: a well-differentiated steroid-responsive endometrial cell line with characteristics of luminal epithelium. Biol Reprod. 2006;75:387–94.
Castelbaum AJ, Ying L, Somkuti SG, Sun J, Ilesanmi AO, Lessey BA. Characterization of integrin expression in a well differentiated endometrial adenocarcinoma cell line (Ishikawa). J Clin Endocrinol Metab. 1997;82:136–42.
Hey NA, Li TC, Devine PL, Graham RA, Saravelos H, Aplin JD. MUC1 in secretory phase endometrium: expression in precisely dated biopsies and flushings from normal and recurrent miscarriage patients. Hum Reprod. 1995;10:2655–62.
Aplin JD, Hey NA, Graham RA. Human endometrial MUC1 carries keratan sulfate: characteristic glycoforms in the luminal epithelium at receptivity. Glycobiology. 1998;8:269–76.
Meseguer M, Aplin JD, Caballero-Campo P, O’Connor JE, Martín JC, Remohí J, Pellicer A, Simón C. Human endometrial mucin MUC1 is up-regulated by progesterone and down-regulated in vitro by the human blastocyst. Biol Reprod. 2001;64:590–601.
Thathiah A, Brayman M, Dharmaraj N, Julian JJ, Lagow EL, Carson DD. Tumor necrosis factor alpha stimulates MUC1 synthesis and ectodomain release in a human uterine epithelial cell line. Endocrinology. 2004;145:4192–203.
Horne AW, White JO, Margara RA, Williams R, Winston RM, Lalani E. MUC 1: a genetic susceptibility to infertility? Lancet. 2001;357:1336–7.
Horne AW, Lalani EN, Margara RA, Ryder TA, Mobberley MA, White JO. The expression pattern of MUC1 glycoforms and other biomarkers of endometrial receptivity in fertile and infertile women. Mol Reprod Dev. 2005;72:216–29.
Santos F, Hyslop L, Stojkovic P, Leary C, Murdoch A, Reik W, Stojkovic M, Herbert M, Dean W. Evaluation of epigenetic marks in human embryos derived from IVF and ICSI. Hum Reprod. 2010;25:2387–95.
Lagow EL, Carson DD. Synergistic stimulation of MUC1 expression in normal breast epithelia and breast cancer cells by interferon-gamma and tumor necrosis factor-alpha. J Cell Biochem. 2002;86:759–72.
Rout UK, Saed GM, Diamond MP. Transforming growth factor-beta1 modulates expression of adhesion and cytoskeletal proteins in human peritoneal fibroblasts. Fertil Steril. 2002;78:154–61.
Kapiteijn K, Koolwijk P, van der Weiden RM, van Nieuw AG, Plaisier M, van Hinsbergh VW, Helmerhorst FM. Human embryo-conditioned medium stimulates in vitro endometrial angiogenesis. Fertil Steril. 2006;85(Suppl 1):1232–9.
Pirtea P, de Ziegler D, Ayoubi JM. Endometrial receptivity in adenomyosis and/or endometriosis. Fertil Steril. 2023;119:741–5.
Salmeri N, Gennarelli G, Vanni VS, Ferrari S, Ruffa A, Rovere-Querini P, Pagliardini L, Candiani M, Papaleo E. Concomitant Autoimmunity in Endometriosis Impairs Endometrium-Embryo Crosstalk at the Implantation Site: A Multicenter Case-Control Study. J Clin Med. 2023;12:3557.
Acknowledgements
The authors thank patients included in the study. AJ acknowledges the Dr. TMA Pai PhD Fellowship from the Manipal Academy of Higher Education (MAHE). Help from Dr Dipty Singh, Scientist E, Confocal facility, ICMR-NIRRCH is gratefully acknowledged.
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal This work was partly supported by research grant from the Indian Council of Medical Research (ICMR # 5/10/FR/8/2014-RCH).
Author information
Authors and Affiliations
Contributions
SKA and GS planned and designed the study. AJ and IM were responsible for the data collection. AJ, VLR, IM analysed the data. SKA, GS drafted the article, while all authors critically revised the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Competing interest
None.
Compliance with ethical standards
The study was approved by the Institutional Ethics committee (IEC) of the Kasturba Hospital of Manipal Academy of Higher Education and informed written consent was obtained from all the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jijo, A., Munshi, I., Uppangala, S. et al. Secretomes from Conventional Insemination and Intra-Cytoplasmic Sperm Injection Derived Embryos Differentially Modulate Endometrial Cells In Vitro. Reprod. Sci. 31, 2080–2091 (2024). https://doi.org/10.1007/s43032-024-01504-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-024-01504-z
Keywords
Profiles
- Satish Kumar Adiga View author profile