Abstract
Purpose
Determine if the SPIKES method was associated with less distress and more compassion than current modes of delivering negative pregnancy test results to patients undergoing in vitro fertilization.
Methods
Twenty-seven nurses from two centers were randomized to use the modified SPIKES script or continue their standard of care; 136 patients with a negative hCG following embryo transfer were included. SPIKES nurses received 1 h of training by a study psychologist; nurses in the control group were instructed to deliver the news as done previously. Patients who underwent embryo transfer and received a call by a participating nurse with a negative test result received an email invitation on the following day.
Results
Control patients reported significantly less distress than SPIKES patients; 33% of SPIKES patients reported that they had felt “extremely sad,” compared to 15.2% of the control patients (p = 0.01). Perceived compassion did not differ between the groups (all p ≥ 0.22).
Conclusion
Patients who received a negative pregnancy test result from the nurses who received a brief training and a script on how to deliver bad news via the modified SPIKES protocol reported significantly more distress than patients receiving negative results from nurses utilizing their standard of care. It is unclear whether a modified SPIKES method to deliver negative pregnancy test results will benefit patients undergoing in vitro fertilization.
Trial registration
Clinical trials.gov NCT04917445.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Data availability
Data can be available upon request.
References
Maynard DW. On “Realization” in everyday life: the forecasting of bad news as a social relation. Am Sociol Rev. 1996;61:109. https://doi.org/10.2307/2096409.
Ptacek JT, Ptacek JJ. Patients’ perceptions of receiving bad news about cancer. JCO. 2001;19:4160–4. https://doi.org/10.1200/JCO.2001.19.21.4160.
Schmid Mast, Kindlimann A, Langewitz W. Recipients’ perspective on breaking bad news: how you put it really makes a difference. Patient Educ Couns. 2005;58:244–251.
Ford S, Fallowfield L, Lewis S. Doctor-patient interactions in oncology. Soc Sci Med. 1996;42:1511–9.
García D, Bautista O, Venereo L, Coll O, Vassena R, Vernaeve V. Training in empathic skills improves the patient-physician relationship during the first consultation in a fertility clinic. Fertil Steril. 2013;99:1413–8.
Quinn GP, Bowman Curci M, Reich RR, Gwede CK, Meade CD, Vadaparampil ST. Impact of a web-based reproductive health training program: ENRICH (educating nurses about reproductive issues in cancer healthcare). Psychooncology. 2019;28:1096–101.
Gameiro S, Boivin J, Dancet E, De Klerk C, Emery M, Lewis-Jones C, et al. ESHRE guideline: routine psychosocial care in infertility and medically assisted reproduction - a guide for fertility staff. Hum Reprod. 2015;30:2476–85.
ASRM Ethics Committee. Fertil Steril. 2019;111:659–63. https://doi.org/10.1016/j.fertnstert.2019.01.033.
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-a six step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:302–311.
Buckman R, Kason Y. How to break bad news: a guide for health care professionals. Baltimore: Johns Hopkins University Press; 1992.
McFarlane J, Riggins J, Smith TJ. SPIKE: a six-step protocol for delivering bad news about the cost of medical care. J Clin Oncol. 2008;26:4200–4.
Tuffrey-Wijne I. A new model for breaking bad news to people with intellectual disabilities. Palliat Med. 2013;27:5–12.
Leone D, Menichetti J, Barusi L, Chelo E, Costa M, De Lauretis L, et al. Breaking bad news in assisted reproductive technology: a proposal for guidelines. Reprod Health. 2017;14:1–10.
Mirza RD, Ren M, Agarwal A, Guyatt GH. Assessing patient perspectives on receiving bad news: a survey of 1337 patients with life-changing diagnoses, AJOB Empir. Bioeth 2018; 1–8. https://doi.org/10.1080/23294515.2018.1543218.
Teike FL, Cantin B. Breaking bad news: “EPICES”, a French style as a learning method. Rev Med Suisse. 2011;7:85–7.
Dean A, Willis S. The use of protocol in breaking bad news: evidence and ethos. Int J Palliat Nurs. 2016;22:265–71.
von Blanckenburg P, Hofmann M, Rief W, Seifart U, Seifart C. Assessing patients’ preferences for breaking bad news according to the SPIKES-Protocol: the MABBAN scale. Patient Educ Couns. 2020;103(8):1623–9.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;2009(42):377–81.
Gonzalez-Cabrera M, Ortega-Martinez AR, Martinez-Galiano JM, Hernandez-Martinez A, ParraAnguita L, Frias-Osuna A. Design and validation of a questionnaire on communicating bad news in nursing: a pilot study. Int J Environ Res Pub Health. 2020;17:457.
Bruera E, Palmer JL, Pace E, Zhang K, Willey J, Strasser F, Bennett MI. A randomized controlled trial of physician postures when breaking bad news to cancer patients. Palliat Med. 2007;21:501–5.
Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17:371–9.
Freeman EW, Boxer AS, Rickels K, Tureck R, Mastroianni L. Psychological evaluation and support in a program of in vitro fertilization and embryo transfer. Fertil Steril. 1985;43(1):48–53.
Domar AD, Zuttermeister PC, Friedman R. The psychological impact of infertility: a comparison with patients with other medical conditions. J Psychosom Obstet Gynaecol. 1993;14(Suppl):45–52.
Vaughan DA, Shah JS, Penzias AS, Domar AD, Toth TL. Infertility remains a top stressor despite the COVID-19 pandemic. Reprod Biomed Online. Published online June 2020:S147264832030314X. https://doi.org/10.1016/j.rbmo.2020.05.015.
Cousineau TM, Domar AD. Psychological impact of infertility. Best Pract Res Clin Obstet Gynaecol. 2007;21:293–308.
Chen TH, Chang SP, Tsai CF, Juang KD. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Hum Reprod. 2004;19:2313–8.
Verhaak CM, Smeenk JMJ, Evers AWM, Kremer JAM, Kraaimaat FW, Braat DDM. Women’s emotional adjustment to IVF: a systematic review of 25 years of research. Human Reprod. 2007;13:27–36.
Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist O, Sundström Poromaa I. Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Human Reprod. 2008;23:1056–63.
Pasch LA, Holley SR, Bleil ME, Shehab D, Katz PP, Adler NE. Addressing the needs of fertility treatment patients and their partners: are they informed of and do they receive mental health services? Fertil Steril. 2016;106:209–15.
Ramezanzadeh F, Aghssa MM, Abedinia N, et al. A survey of relationship between anxiety, depression and duration of infertility. BMC Womens Health. 2004;4(1): 9. https://doi.org/10.1186/14726874-4-9.
Maroufizadeh S, Karimi E, Vesali S, Omani SR. Anxiety and depression after failure of assisted reproductive treatment among patients experiencing infertility. Int J Gynaecol Obstet. 2015;130:253–6.
Crawford NM, Hoff HS, Mersereau JE. Infertile women who screen positive for depression are less likely to initiate fertility treatments. Hum Reprod. 2017;32(3): 582587.
Gameiro S, Boivin J, Peronace L, Verhaak CM. Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Hum Reprod Update. 2012;18:652–69.
Gameiro S, Boivin J, Domar A. Optimal in vitro fertilization in 2020 should reduce treatment burden and enhance care delivery for patients and staff. Fertil Steril. 2013;100:302–9.
Domar AD, Rooney K, Hacker MR, Sakkas D, Dodge LE. Burden of care is the primary reason why insured women terminate in vitro fertilization treatment. Fertil Steril. 2018;109:1121–6.
Palmer-Wackerly AL, Voorhees HL, D’Souza S, Weeks E. Infertility patientprovider communication and (dis)continuity of care: an exploration of illness identity transitions. Patient Educ Couns. 2019;102:804–9.
Dancet EAF, Van Empel IWH, Rober P, Nelen WLDM, Kremer JAM, Dhooghe TM. Patient-centred infertility care: a qualitative study to listen to the patients voice. Hum Reprod. 2011;26:827–33.
Gameiro S, Canavarro M, Boivin J. Patient centred care in infertility health care: direct and indirect associations with wellbeing during treatment. Patient Educ Couns. 2013;93:646–54.
Malin M, Hemmink E, Räikkönen O, Sihvo S, Perälä ML. What do women want? Women’s experiences of infertility treatment. Soc Sci Med. 2001;53:123–33.
Schmidt L, Tjørnhøj-Thomsen T, Boivin J, Nyboe AA. Evaluation of a communication and stress management training programme for infertile couples. Patient Educ Couns. 2005;59:252–62. 12.
Ussher JM, Parton C, Perz J. Need for information, honesty and respect: patient perspectives on health care professionals communication about cancer and fertility. Reprod Health. 2018;2018(15):2. https://doi.org/10.1186/s12978-017-0441-z.
Mosconi L, Crescioli G, Vannacci A, Ravaldi C. Communication of diagnosis of infertility: a systematic review. Front Psychol. 2021;12: 615699. https://doi.org/10.3389/fpsyg.2021.615699.
Goncalves JJ, Nascimento TGLd, Pereira MMdM, Moreira EB. Changes in communicating bad news in the context of COVID-19: adaptations to the SPIKES protocol in the context of telemedicine. Front Psychiatr. 2020;11:599722.
Acknowledgements
The authors would like to thank Sharon Edwards, RN, BSN, and Susan Gordon-Pinnell, RN, BSN, for their assistance with nursing recruitment at Boston IVF. The authors would also like to thank Schuyler Awtrey for her assistance with the preparation of this manuscript.
Funding
This study was funded by the Domar Foundation as well as support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR002541) and financial contributions from Harvard University and its affiliated academic healthcare centers.
Author information
Authors and Affiliations
Contributions
Drs. Domar, Korkidakis, Bortoletto, and Grill participated in study design, execution, analysis, manuscript drafting, and critical discussion. Dr. Hacker and Ms. Gompers participated in study design, analysis, manuscript drafting, and critical discussion. Ms. Gulrajani and Ms. Khodakhah participated in execution, manuscript drafting, and critical discussion. Ms. Rooney participated in study design, execution, manuscript drafting, and critical discussion.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1. SPIKES script
Hi this is [nurse full name], one of the IVF nurses at Cornell/Boston IVF.
May I please speak with [patient full name]
Is now a good time to talk about your test results?
If no
When would be a good time to call back?
If yes
Before we review the results, is there anyone else you would like to add to the call?
Delivery:
Have you taken a home pregnancy test before getting your results today?
If yes
Unfortunately, the blood work confirmed that you are not pregnant. I am so sorry I know this is not the result you hoped for.
If no
I am so sorry to have to share this information with you. Your pregnancy test came back negative. I know this is not the result you hoped for.
Questions
Would you like to know all of the details such as your beta hCG level or would you prefer to take time to digest the information?
If yes
(Give test results & proceed to “if no” step below)
If no
I know this is disappointing information—what questions do you have so far?
Checking in with patient
How are you doing?
How are you feeling?
It is understandable that you are feeling [whatever feeling patient expressed].
I can see how upsetting this is to you and I wish the news were better.
Next Steps
[Discuss next steps with patient – including what to do about medication and setting up follow-up time with their doctor].
I’m sure you will think of many more questions.
When you do, write them down and you can review them with our doctor during your follow up appointment or feel free to reach out to me.
Wrap Up
Before I go, do you have someone to talk to and support you after we hang up?
You don’t have to deal with this alone. We have counselors on staff who can help you process this information and support you.
We have a whole team on your side to help with next steps when and if you are ready.
Okay, bye [patient first name].
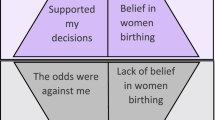
Appendix 2



Appendix 3. Email invite to patients
Dear [insert patient name],
We are constantly working to make your care here as patient-centered as possible. One of the aspects of care that we are contemplating changing is the way that the news of a negative pregnancy test is delivered.
Would you be willing to complete two brief research questionnaires? All answers are completely anonymous and non-identifying, neither your physician nor nurse will know that you completed this questionnaire.
Your answers will be used to help study the most compassionate way to deliver disappointing information.
If you agree to support us in this quick research project, please click on this link: [insert link].
Thank you,
Research Assistant
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Domar, A.D., Korkidakis, A., Bortoletto, P. et al. The impact of an adapted SPIKES protocol vs routine care in the delivery of bad news to IVF patients: an exploratory pilot multicenter randomized controlled trial. J Assist Reprod Genet 41, 2367–2377 (2024). https://doi.org/10.1007/s10815-024-03198-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03198-3